About Pacific Health Care Organization
Pacific Health Care Organization, Inc. (PHCO) operates as a workers' compensation cost containment specialist.

The company engages in providing a range of services principally to California employers and claims administrators. Medex Healthcare, Inc. (Medex) is a wholly owned subsidiary of the company. Medex is in the business of managing and administering both Health Care Organizations ('HCOs') and Medical Provider Networks ('MPNs') in the state of California. Medex also offers Workers' Compensation carve-out services, Medicare set-asides and expert witness testimony.
In February 2012, the company incorporated MMM (Medex Medical Management, Inc.) in the state of Nevada, as a wholly owned subsidiary of the company. MMM is responsible for overseeing and managing medical case management services. In March 2011, the company incorporated MMC (Medex Managed Care, Inc.) in the state of Nevada, as a wholly owned subsidiary of the company. MMC oversees and manages the company's utilization review, medical bill review services, and lien representation services.
The company offers an integrated and layered array of complimentary business solutions that enable the company's customers to better manage their employee workers' compensation-related healthcare administration costs. The company is constantly looking for ways to expand the suite of services the company can provide its customers, either through strategic acquisitions or organic development.
The company's services focus on ensuring timely medical treatment to reduce the claim duration and medical treatment costs.
The company's services include providing customers access to its HCOs and MPNs. The company also provides medical case management, medical bill review, utilization review, workers' compensation carve-outs and Medicare set-aside services. Complementary to these services, the company also provides lien representation and expert witness testimony. The company offers its services as a bundled solution, as standalone services, or as add-on services.

The company's core services focus on reducing medical treatment costs by enabling the company's customers to have control and oversight of the medical treatment of their injured employees to ensure treatment is timely and appropriate. This control is primarily obtained by participation in one of the company's medical provider networks. The company holds several government-issued licenses to operate medical provider networks. Through Medex, the company holds two of the total of four licenses issued by the state of California to establish and manage HCOs within the state of California. The company also holds approvals issued by the state of California to act as an MPN and administer 27 MPNs. The company's HCO and MPN programs provide the company's customers with provider networks within which the customer has some ability to direct the administration of the claim. This is designed to decrease the incidence of fraudulent claims and disability awards and ensure injured employees receive the necessary back-to-work rehabilitation and training they need. The company's medical bill and utilization review services provide oversight of medical billing and treatment requests, and the company's medical case management keeps workers' compensation claims progressing to a resolution and assures treatment plans are aligned from a medical perspective.
The company's customers include self-administered employers, insurers, third party administrators, municipalities, and others. The company's principal customers are companies with operations located in the state of California where the cost of workers' compensation insurance is a critical problem for employers, though the company processes medical bill reviews, utilization reviews and provide medical case management in several other states. The company's provider networks, which are located only in California, are composed of providers experienced in treating worker injuries.
Health Care Organizations
An HCO is a network of health care providers specializing in the treatment of workplace injuries and in back-to-work rehabilitation for the company's customers' injured employees. HCOs provide injured employees with a network of health care providers in the event of a workers' compensation injury, while providing their employer (the company's customer) control over medical treatment and costs. In most cases, the company's HCOs give the employer up to 180 days of medical control in an HCO within which the employer can direct the administration of the claim.
The company's two HCO licenses (respectively referred to as 'Medex HCO' and 'Medex 2 HCO') allow the company to provide comprehensive medical provider networks throughout California. The company's HCO networks are composed of medical providers experienced in treating worker injuries. The company has contracted with approximately 5,500 and 6,700 individual medical providers and clinics for Medex HCO and Medex 2 HCO, respectively, as well as hospitals, and rehabilitation centers. The company's customers select one of the Medex HCO networks to enroll their employees in based on the medical groups in the network. During initial enrollment and during the period of re-enrollment, the company's customers' employees have the option to opt-out of the HCO by predesignating their primary care physician to manage a workplace injury. If the employee opted out and is later injured on the job, their primary care physician would be authorized to oversee their medical care. Otherwise, the employer would be able to select the provider to oversee their medical care.
The company continually reviews and updates its networks with provider additions and removals based on feedback from internal operations, the company's customers and their claims administrators. All the company's network providers' credentials are reviewed and vetted by Medex.
The company's HCO networks are required to be recertified every three years. The Medex HCO has been recertified through March 15, 2025 and the Medex 2 HCO through October 9, 2024. HCO guidelines impose certain medical oversight, reporting, information delivery and usage fees on HCOs. These requirements increase the administrative costs and obligations on HCOs compared to MPNs, although the obligations and cost differentials between the two types of organizations have been narrowing over the past few years.
Medical Provider Networks
Unlike the company's HCOs, its MPNs do not require the company's customers to pay annual enrollment fees, nor do they require the company's customers to comply with annual enrollment notice delivery requirements. As a result, there are fewer administrative costs to customers associated with an MPN program. This allows the company's MPNs to market their services at a lower cost to employers than the company's HCOs. For this reason, many customers may opt to use the MPN even though it provides customers fewer rights to control medical treatment of employee injury claims.
The company has received approval for and administers 27 MPNs. Customers can choose between two of the company's off-the-shelf MPNs, which serve as stand-alone networks or the foundation for the customer to customize their own MPN, in which they can add or remove specific providers or clinics. Each MPN must be reapproved every four years for each customer based on the date the MPN was approved by the California Division of Workers' Compensation.
HCO and MPN Hybrid Offering
As a licensed HCO and approved MPN, in addition to offering HCO and MPN programs, the company is also able to offer its customers a combination of the HCO and MPN programs. Under this program, a customer can enroll its employees in the company's HCO program, and then prior to the expiration of the 180-day treatment period under the HCO program, the customer (the employer) can then enroll their injured employees into the company's MPN program to keep the medical care within their network of providers. This allows the company's customers to take advantage of both programs, which is what the company's HCO customers typically do. To the company's knowledge, Medex is the only entity in California offering this hybrid program.
Medical Case Management
Medical case management oversees the injured employees' medical treatment to ensure that it progresses to a resolution and assures treatment plans are aligned from a medical perspective. Medical case management is a collaborative process that assesses, evaluates, coordinates, implements and monitors medical treatment plans and the options and services required to get the injured employee back to work. Medical case managers act as liaisons between the injured employee, claims adjuster, medical providers, and attorneys to achieve optimal results for the injured employee and their employer.
The company's medical case management services are performed by nurses who are credentialed by the state and have expertise in various clinical areas and backgrounds in workers' compensation matters. This combination allows the company's nurses the opportunity to facilitate medical treatment while understanding the nuances of workers' compensation up to and including litigation. By utilizing these services, the company's customers can ensure that the injured employee receives quality medical treatment in a timely and appropriate manner to help the employee return to work and close the workers' compensation claim.
Medical Bill Review
Medical bills are one of the biggest expenses that an employer's workers' compensation insurance company must pay for. To curtail these expenses, the company's customers utilize its medical bill review services to review medical bills for services rendered to an injured employee. The company provides professional analysis of medical provider services and equipment billing to ascertain proper reimbursement. The company's review of medical bills includes coding review and re-bundling, confirming that the services are customary and reasonable, fee schedule compliance, out-of-network bill review, pharmacy review, and preferred provider organization repricing arrangements. While some states have adopted fee schedules, which regulate the maximum allowable fees payable under workers' compensation for procedures performed by a variety of health treatment providers, many procedures are not covered by fee schedules and are still subject to review and negotiation.
Medical bill review services can result in significant claims savings. The company's medical bill services are primarily within the state of California, but the company processes medical bill review in several other states. Out of state medical bill reviews typically are the result of an injured California employee moving to a different state, but who still requires medical care under an open workers' compensation claim.
Utilization Review
Utilization review is required by law in all states for workers' compensation claims. Utilization review evaluates the medical necessity of proposed treatment by comparing medical treatment requests against accepted medical guidelines. Its purpose is to serve as a safeguard against payor liability for medical costs that are not medically appropriate or approved by the relevant medical and legal authorities. Reviews of medical treatment requests are conducted at the appropriate qualification level for the request by a nurse, peer-to-peer provider, a specialist or a medical director and within the timelines set by the relevant laws and regulations.
The company's utilization review services provide an electronic intake of medical treatment requests, collection and review of the submitted documentation required for processing, and submission to the appropriately qualified reviewer for approval, modification, denial, or request for more information for the requested treatment. Once a determination is made, the company processes the request and notify all the stakeholders in the injured employee's claim within the regulated timeframe.
Medicare Set-aside
Medicare set-aside services for workers' compensation claims is a financial agreement that allocates a portion of a workers' compensation settlement to pay for future medical services related to the work-place injury, illness, or disease. The purpose of the set-aside arrangement is to provide funds to the injured party to pay for future medical expenses that would not be covered by Medicare. This program affords the company's customers an effective way to overcome complications after settlement and avoids unnecessary costs attached to the claim.
Workers' Compensation Carve-outs
Certain employers can opt out of the standard workers' compensation regulatory dispute resolution scheme through carve-out agreements that comply with state statutory and regulatory requirements. More specifically, carve-out agreements permit employers and employees to establish alternative dispute resolution arrangements to resolve disputes in the context of workers' compensation. These carve-out agreements are made between employers and the collective bargaining units representing the employer's covered employees.
Utilizing the company's knowledge of the friction in the California workers' compensation system, and the objectives of employers and the unions, the company assists in guiding the negotiation of legal agreements for the implementation of workers' compensation carve-outs for California customers and provide services that reflect the parties' agreement with regard to alternative dispute resolution arrangements. Under such carve-out agreements certain customers can access the company's HCOs, MPNs and medical case management program.
Lien Representation
When a worker is injured in the scope of employment the employer is required to provide workers' compensation benefits, including medical treatment. If the medical treatment is not paid because the services were not authorized, or if the provider disputes the amount of reimbursement, the provider may file a lien against the workers' compensation claim, which must be resolved by the employer. In these cases, the company provides its customers lien representation services that include negotiation through litigation and petitions for reconsideration.
Expert Witness Testimony
As an ancillary service to the company's HCO and MPN services, the company provides expert witness testimony before the California Workers Compensation Appeals Board. The fees the company charges for this service include reimbursement of expert witness fees and travel and lodging expenses for all HCO customers except for one, whose fees are included in their monthly global fee.
Marketing and Customers
The company provides services to virtually any size employer in the state of California, as well as insurers, third party administrators, self-administered employers, municipalities, and other industries. The company also provides some customers utilization review and/or utilization management, medical case management, and medical bill review services outside the state of California, typically to employees who have suffered a workplace injury in California and then relocated to another state.
The company's marketing and sales efforts focus primarily on customer referrals, conference presentations and responding to requests for proposals. The company services both local and national accounts, however, with an emphasis on California focused markets. The company's sales and marketing activities are conducted by account managers with the assistance of the company's executive team members. The company does not market its services outside the state of California.
The company's services can be integrated to allow for partial or full bundling of services and sharing of information that create efficiencies to further reduce the costs of claims. For example, the company's bundled services have allowed some customers to achieve up to a 70% reduction in the cost of injury claim resolution while maintaining superior treatment for their injured employees. The cost to the company's customers for its bundled services is generally the same as if the services were purchased individually.
Governmental Regulation
MMC is required to be accredited by the independent, nonprofit accreditation entity, Utilization Review Accreditation Commission ('URAC'), in California to perform utilization review and is subject to a routine investigation by the state of California every five years. MMC has received full Utilization Management Accreditation for Workers' Compensation as a Utilization Review Organization ('URO') from URAC.
History
The company was incorporated under the laws of the state of Utah in 1970. It was formerly known as Clear Air, Inc. and changed its name to Pacific Health Care Organization, Inc. in 2001.
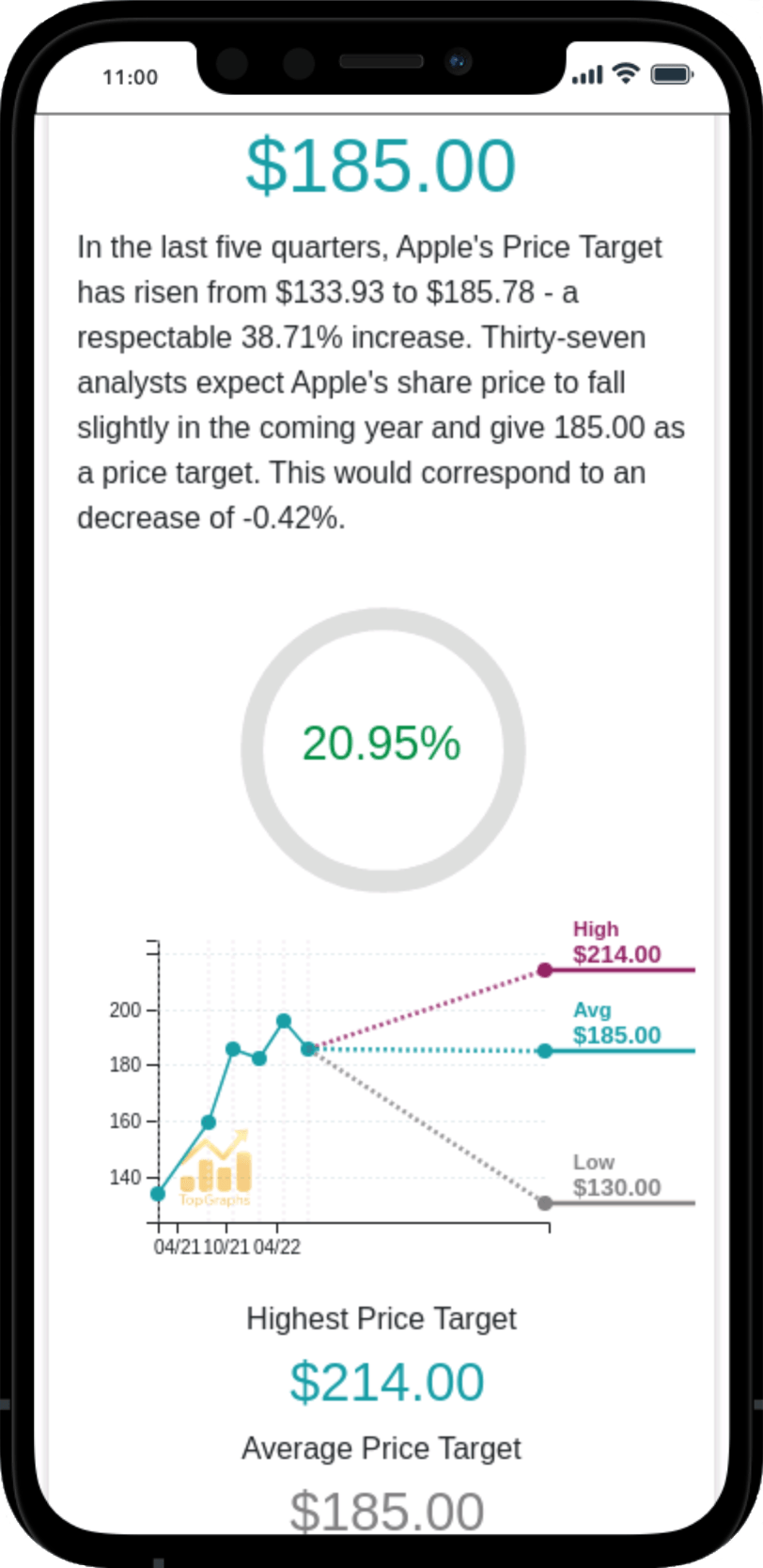
 Stock Value
Stock Value