About R1 RCM
R1 RCM Inc. is a leading provider of technology-driven solutions that transform the financial performance and patient experience for health systems, hospitals, and physician groups. The company's scalable operating models complement a healthcare organization's infrastructure, driving sustainable improvements to net patient revenue (NPR) and cash flows while driving revenue yield, and enhancing the patient experience.

The company served over 3,700 hospitals, including 93 of the top 100 health systems, and over 30,000 physicians as of December 31, 2023. The company's dedicated focus on optimizing revenue cycle performance enables its customers to focus on their patients and communities. The company offers a comprehensive suite of solutions that covers all areas of the revenue cycle and employs a large team of revenue cycle experts.
The company delivers solutions to customers through leading-edge technology, proprietary expertise, intellectual property (IP), global scale, and operational excellence - key elements to driving durable financial performance across the revenue cycle.
Comprehensive and Flexible Offerings for Healthcare Providers
The company's flexible partnership models are intentionally designed to meet the unique needs of the providers the company serves. The company's commitment as an accountability partner with the ability to deliver multiple integrated solutions at scale allows it to engage with customers in a manner that aligns with their objectives. The company's commitment to serving a diverse range of healthcare providers is demonstrated in its flexible partnership models, from modular solutions to full end-to-end revenue cycle operating partnerships.
Operating Partnership/End-to-End Solutions: For organizations seeking comprehensive support across the entire revenue cycle, the company's operating partnership model manages multiple aspects of the revenue cycle, enabling hospital and physician customers to realize financial leverage and revenue improvement. Under this partnership model, the company assumes full responsibility of all or select revenue cycle phases to deliver scalable, accelerated, and sustainable financial results across all settings of care and payment models, customized for health systems and physician groups.

Modular Solutions: For organizations looking to accelerate, optimize, and navigate revenue recovery, the company offers modular solutions, which can be purchased individually or bundled and are designed to deliver results in key revenue cycle areas. Under this focused and flexible partnership approach, the company addresses specific challenges of the revenue cycle. This customized approach promotes enhanced revenue performance in areas that matter most for health systems, hospitals, and physician groups. These solutions are grouped into five categories that address unique healthcare provider challenges and drive value in specific areas of the revenue cycle:
Functional Partnership: Functional outsourcing solutions drive improvements across targeted revenue cycle areas for hospital and physician group customers. These modular solutions are for organizations requiring focused support in specific areas.
Revenue Recovery: Modular solutions to fast-track payer and patient cash collections with proprietary technology backed by the company's experience in aged, complex and clinically challenged claims and denials. For these modular solutions related to back-end payment collections, it applies automation and AI to an otherwise labor-intensive process.
Revenue Optimization: Modular solutions to uncover missed or underreported revenue with the company's comprehensive payment review expertise designed to identify areas that may be missed by other internal processes.
Clinical Integrity: Modular solutions to improve documentation and coding accuracy to maximize earned revenue for the services provided. The company's clinical and auditing experts support these modular solutions.
Regulatory Navigation: Modular, compliance-first solutions to optimize government reimbursement accuracy, maximize pharmacy savings, and ensure compliance with the help of the company's elite team of industry specialists.
Drivers of RCM Impact Delivered by End-to-End and Modular Solutions
Across its end-to-end and modular solutions, the company seeks to improve its customers' revenue cycles and processes using a variety of techniques including:
Deploying Proprietary Technology and Algorithms: The company's systems are designed to streamline work processes through use of proprietary algorithms that focus revenue cycle staff efforts on those accounts deemed to have the greatest potential for improving net revenue yield. The company adjusts its proprietary, predictive algorithms to reflect changes in payer and patient behavior based upon its cumulative knowledge and experience gained from servicing its customer base. As new customers are added and payer and patient behavior changes, the information the company uses to create its algorithms expands, increasing the accuracy, reliability, and value of such algorithms.
Deploying Analytical and Operational Excellence: The company draws on the experience that it has gained from working with some of the top healthcare provider systems in the U.S. to train its customers' staff about new and innovative RCM practices. In addition to core key performance indicators that provide visibility into revenue cycle performance, the company provides value-added analytics that expose notable changes in payer behavior and accounts requiring escalation, as well as provide visibility into performance variances. The company's deep analytical insights allow it to run predictive modeling and trend analysis in order to anticipate potential challenges, identify areas for improvement and guide strategic decision-making that impact revenue cycle performance.
Increasing Revenue Capture and Preventing Future Losses: The company's robust platform integrates with provider systems to identify revenue optimization areas, while exposing root cause issues requiring intervention.
Leveraging its Global Business Services Operations: Examples of services that can be completed at the company's global business services operations include financial clearance functions like pre-registration and insurance verification, coding and charge compliance, cash posting, reconciliation of payments to billing records, and patient and payer follow-up.
In addition, certain other techniques are specific to the company's end-to-end solutions or modular solutions. Additional techniques utilized in delivering the company's end-to-end solutions include the following:
Sophisticated and Comprehensive Onboarding Process: Anchored by over 100 dedicated experts, the company's cross-functional onboarding team collaboratively works with its customers to stabilize and elevate overall performance. The company's onboarding experience includes change management, employee transition, operational and compliance assessment, as well as technology deployment - elements to assist in a seamless transition and set the stage for sustained revenue cycle success.
Comprehensive Patient and Payer Information Collection: The company focuses on gathering comprehensive patient information and validating insurance eligibility and benefits so patient care services can be recorded and billed to the appropriate parties. For scheduled healthcare services, the company educates patients as to their potential financial responsibilities before receiving care. Through its systems, the company maintains an automated electronic scorecard which measures the efficiency of up-front data capture, authorization, billing, and collections throughout the life cycle of any given patient account. The company's dedicated performance management team analyzes these scorecards in the aggregate, and the results are used to help improve workflow processes and operational decisions for its customers.
Improving Claim Filings and Collections: Through its proprietary technology and process expertise, the company identifies, for each patient encounter, the estimated amount due from the patient and the amount its customer should receive from a payer based on the customer's contracts with payers or the patient's policy.
Alternative Payment Sources Identification and Patient Balance Resolution: The company uses various methods to find payment sources for uninsured patients and reimbursement for services not covered by payers. The company's patient financial screening technology and methodologies often identify federal, state, or private grant sources to help pay for healthcare services. These techniques are designed to ease the financial burden on uninsured or underinsured patients, increase the percentage of patient bills that are actually paid, and improve the total amount of reimbursement received by its customers. For balances that remain due from patients, the company provides financing and payment options tailored to the patients' unique circumstances, minimizing their financial burden and increasing yield for its customers.
Additional techniques utilized in delivering the company's modular solutions include the following:
Auditors Accelerate Revenue Capture and Ensure Compliance Through the Application Of Automation and AI: With its collective experience across the financial and clinical side of healthcare, the company's revenue cycle experts bring a wealth of industry knowledge to its engagements. Leveraging proprietary technology to rapidly identify revenue opportunities, its auditors help to ensure that revenue is captured accurately and in compliance with the latest regulations. They serve as strategic partners, identifying opportunities for optimization, while guiding the company's customers toward sustained financial success.
Comprehensive Dataset to Expose and Prioritize Revenue Opportunities: The company's approach to a standardized data specification across all customers promotes consistency, interoperability and efficiency in data and revenue cycle performance. By collecting comprehensive patient billing and reimbursement data of 93 of the top 100 health systems, the company is able to identify macro-trends that impact healthcare providers across the nation, and also identifies rapid revenue collection opportunities for its customers.
Segment
The company views its operations and manages its business as one segment. All of the company's net services revenue and trade accounts receivable are derived from healthcare providers domiciled in the U.S.
Customers
The company's customers typically are healthcare providers, including health systems, hospitals, and physician groups.
Hospital systems affiliated with Ascension Health (Ascension) have accounted for a significant portion of the company's net services revenue each year since its formation. For the year ended December 31, 2023, net services revenue from healthcare providers affiliated with Ascension represented 40% of its total net services revenue.
Sales and Marketing
The company's customer acquisition process leverages traditional and non-traditional techniques to inform the marketplace of its complete range of solutions and its ability to meet customers where they are on their RCM journey. For new customer acquisitions, broad outreach and interest are transitioned into selling opportunities through a highly targeted sales and marketing pipeline management process backed by demand generation programs that communicate its differentiation of purpose-built technology and deep expertise. Initial interaction with a prospective health system typically begins with a key decision maker and includes a comparison of the potential customer's historical and projected results versus a standardized improvement model. Existing customer expansion sales opportunities are initiated through regular communications related to existing operations or general dialogue around business challenges the customer is facing. For both new and existing customer acquisitions, the next step in the sales process is a detailed assessment of the prospect's existing operations versus its model and a review of the potential opportunities to improve revenue cycle performance.
Operating Partnership: The company's sales process for RCM managed services partnership agreements typically lasts from six to 18 months from the introductory meeting to the agreement's execution.
Modular Solutions: The company's sales process for its modular solutions typically lasts two to six months. Because its modular solutions act as both comprehensive and complementary options in various stages of the revenue cycle, customers have the freedom to selectively consider any of the company's offerings on a standalone basis or in conjunction with one another, taking advantage of like datasets and grouping implementation efforts to create a customized deployment.
Technology and Products
Proprietary Software Suite
The company's integrated suite of RCM technology provides a layer of analytics, rules processing, and workflow capabilities that interface with provider systems to optimize process efficiency and effectiveness. These technologies power the detection of defects on patient accounts and enable staff workflow at point of service areas, customer sites, and the company's global business services operations. The company's technology suite includes, but is not limited to, the following capabilities:
The company's cloud-based platform has the architecture and ability to process large volumes of demographic, clinical, and financial data from over 550 million patient encounters annually and the flexibility to ingest different types of data from numerous disparate sources and customers. The platform applies machine learning algorithms that analyze data and identify revenue cycle inaccuracies and opportunities, then prices those opportunities in accordance with customer-payer contracts. It includes task automation capabilities to enable the company's operators to efficiently complete their workflow and reporting capabilities to provide customer insights.
The company's workflow platform is used in customer central business offices and at its scaled global business services centers for pre-registration, financial clearance, and financial counseling. The platform processes patient accounts through proprietary rules engines tuned to identify defects in demographic data, authorization processes, insurance benefits and eligibility, and medical necessity. The rules engines are also used to calculate patient cost estimates and prior balance accounts receivables. For the uninsured, the platform helps staff triage patients to find coverage for their visit. The company's technology enables staff to work on an exception basis eliminating the need for manual intervention on accounts with no exceptions identified.
The company's patient contact application provides the workflow and data for patient contact center representatives. It enables effective financial discussions with patients on outstanding balances. The platform is integrated into the company's call center, call-routing and auto-dialer capabilities, and facilitates improved outcomes through propriety process and technology approaches.
The company's proprietary contract modeling platform is used to accurately calculate the maximum allowed reimbursement for each claim based upon models of its customer's contract with each payer.
The company's web-based reporting and analytics platform produces over 300 proprietary reports derived from the financial, process, and productivity data that it accumulates as a result of its services, which enable it to monitor and identify areas for improvement in the efficacy of its RCM services.
The company's application platform classifies defects in a proprietary nomenclature and distributes data to back-end teams for follow up and resolution according to standard operating processes. Defects are identified and noted on accounts as they occur. The platform, along with the company's Yield-Based Follow Up application, is designed to power customer patient financial services departments and its global business services.
The company's Physician Advisory Services (PAS) portal allows for the electronic submission, tracking, reviewing, and auditing of patient cases referred to the PAS team. The PAS portal environment is established as a secure site that enables the company to receive patient records from customer case managers and route them to the company's physicians for review. This workflow is supported by an analytics engine within the web portal that provides the company's customers the ability to improve their compliance and workflow with its real-time reporting, dashboards, and worklists.
The company's web-based, mobile responsive application streamlines the interface for patients and physicians within the revenue cycle across all settings of care. It includes enterprise scheduling, self-service appointment management, patient out-of-pocket cost estimation, online pre-registration, financial clearance, authorization automation, and patient payment. The applications for patient and provider self-service are also connected to the company's proprietary rules engines. These rules engines automate the complex tasks necessary to prevent revenue cycle defects and automate the matching of appropriate provider appointment capacity with specific patient needs under any variety of clinical and administrative circumstances.
The company leverages a platform that combines robotic process automation, computer vision/optical character recognition, natural language processing, expert rules/machine learning, workflow integration, and analytics to automate processes across the revenue cycle and manage the digital workforce. This platform allows the company to bring off-the-shelf automation to solve many of the common revenue cycle workflows, while providing the flexibility to efficiently address customer-specific processes. With this technology platform, repetitive transactional processes are automated, delivering operating efficiency and freeing up staff members to focus on higher-order problem solving and higher value-added work. The platform targets a wide range of functions including prior authorization, coding, accounts receivable follow-up, payment posting, and credit balances, among others.
The company's chart manager supports patient medical record deficiency management, by evaluating record completeness and optimizing the chart completion workflow. The application creates an intuitive user experience, queuing work by defect and providing visibility to work in process. It allows hand-offs across departments, and tracking of accountability for chart completion, in order to drive velocity and accuracy of the medical record management and coding processes.
The company offers a solution that supports the end-to-end cash posting function through automation, including the matching of bank deposits to remittance advices, initiating the posting of the remittance advices within a customer's patient accounting system, balancing these transactions, and providing financial reporting. With this technology, unmatched deposits/remittances or unbalanced transactions are able to be worked on an exception-basis.
The company offers a standardized technology solution for performing quality assurance across the various operational verticals. The technology provides audit workflow, statistically-driven sampling, domain-specific audit templates, and staff feedback gathering and alerting functionality.
The company offers a host billing and coding system for hospital-based physicians to facilitate coding, insurance billing, accounts receivable and denials management, patient statements, and cash posting functions.
The company's applications are deployed on a highly-scalable architecture based upon Microsoft and other industry leading platforms. The company offers a common experience for end-users and the consistent look and feel of its applications allows its customers and staff to use its software suite quickly and easily.
Technology Operations
The company's software interacts with its customers' software through a series of real-time and batch interfaces. The company's core RCM and PAS applications are hosted within enterprise-class, industry-leading, third-party data centers located in Dallas, Texas and Ashburn, Virginia. The company's internal financial application suite is hosted in various locations in a U.S.-based cloud model. The third-party partners it uses for hosting are compliant with the Statement on Standards for Attestation Engagements, or SSAE, No. 16, Reporting on Controls at a Service Organization (Service Organization Controls 1). The company has agreements with its hardware and system software suppliers for support 24 hours a day, seven days a week.
Data and information regarding the company's customers' patients reside within the continental U.S. data centers and are encrypted both when transmitted over the internet and at-rest. The company has dedicated links for data replication between its primary and secondary production data centers for resiliency and redundancy. The company also has data backups that occur at appropriate intervals. The company's third-party data centers are designed to withstand many catastrophic events such as blizzards, hurricanes, and power grid anomalies.
Government Regulation
Most of the company's customers are covered entities and the company is a business associate to many such customers under HIPAA as a result of its contractual obligations to perform certain functions on behalf of, and provide certain services to, those customers.
In order to provide the company's covered entity customers with services that involve the use or disclosure of PHI, HIPAA requires the company's customers to enter into business associate agreements with the company.
The company is contractually required to structure and provides its services in a way that supports its customers' HIPAA compliance obligations.
Intellectual Property
The company has been issued eight U.S. patents which expire between 2028 and 2036, upon payment of U.S. Patent maintenance fees. The company has two additional allowed patents (awaiting issuance) and four additional pending U.S. patent applications. Legal standards relating to the validity, enforceability, and scope of protection of patents can be uncertain. The company's eight granted patents or any patents that may be granted in the future from pending or future applications may be opposed, contested, circumvented, designed around by a third party, or found to be invalid or unenforceable.
History
The company was founded in 2003. It was incorporated in Delaware in 2003. The company was formerly known as Healthcare Services, Inc. and changed its name to Accretive Health, Inc. in 2009. Further, the company changed its name to R1 RCM Inc. in 2017.

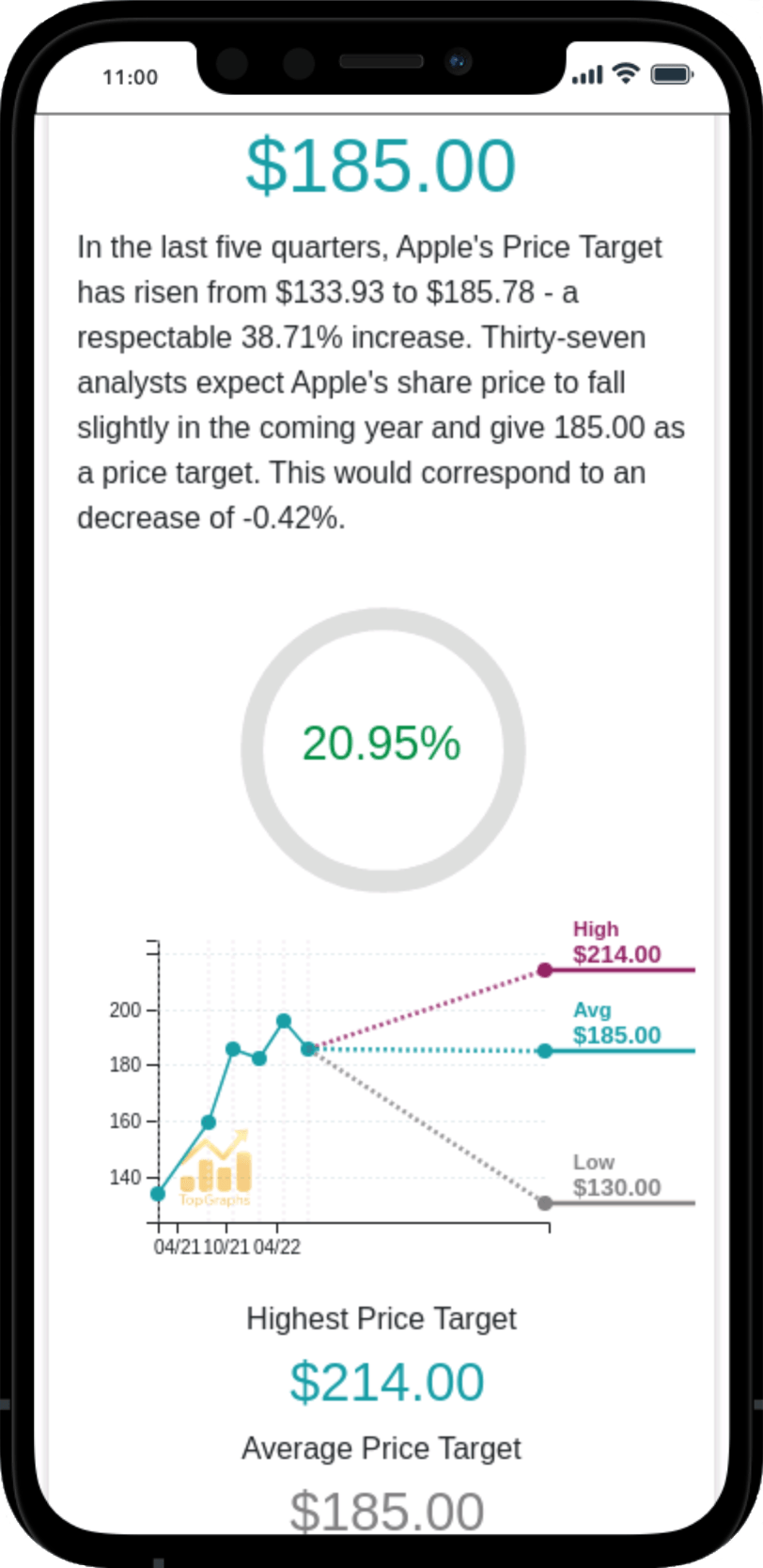
 Stock Value
Stock Value