About Premier
Premier, Inc. (Premier) operates as a technology-driven healthcare improvement company.

The company engages in uniting an alliance of the United States (U.S.) hospitals, health systems and other providers and organizations to transform healthcare.
The company partners with hospitals, health systems, physicians, employers, product suppliers, service providers and other healthcare providers and organizations with the common intention of improving and innovating in the clinical, financial and operational areas of their businesses to meet the demands of a rapidly evolving healthcare industry, and it continues to expand its capabilities to more fully address and coordinate care improvement and standardization in the employer, payer and life sciences markets. With integrated data and analytics, collaboratives, supply chain services, consulting and other services, Premier enables healthcare providers to deliver better care.
The company delivers value through a comprehensive technology-enabled platform that offers critical supply chain services, clinical, financial, operational and value-based care software as a service (SaaS), as well as clinical and enterprise analytics licenses, consulting services, performance improvement collaborative programs, third-party administrator services, access to its centers of excellence program, cost containment and wrap network and digital invoicing and payables automation processes which provide financial support services to healthcare suppliers and providers. Additionally, the company provides some of the various products and services noted above to non-healthcare businesses, including through its direct sourcing activities, as well as continued access to its group purchasing organization (GPO) programs for non-healthcare members whose contracts were sold to OMNIA Partners, LLC (OMNIA).
The company delivers its integrated platform of solutions that address the areas of clinical intelligence, margin improvement and value-based care.
Membership

The company’s membership base includes many of the country’s most progressive and forward-thinking healthcare organizations. As of June 30, 2023, the company’s members included more than 4,350 U.S. hospitals and health systems and approximately 300,000 other providers and organizations. Over 450 individuals, representing approximately 150 of the U.S. hospital members, sit on 29 of its strategic and sourcing committees, and as part of these committees, use their industry expertise to advise on ways to improve the development, quality and value of its products and services.
Segments
The company operates through two business segments, Supply Chain Services and Performance Services.
Supply Chain Services
This segment assists the company’s members and other customers in managing their non-labor expense and capital spend through a combination of products, services and technologies, including one of the largest national healthcare GPO programs in the United States serving acute and continuum of care sites, and providing supply chain co-management, purchased services, direct sourcing and supply chain resiliency activities. Membership in the company’s group purchasing organization (GPO) also provides access to certain supply chain-related SaaS informatics products and the opportunity to participate in its ASCENDrive and SURPASS performance groups. The company’s Supply Chain Services segment consists of the following products and solutions:
Group Purchasing: The company’s portfolio of over 3,300 contracts with over 1,400 suppliers provides its members with access to a wide range of products and services, including medical and surgical products, pharmaceuticals, laboratory supplies, capital equipment, information technology, facilities and construction, food and nutritional products and purchased services (such as clinical engineering and workforce solutions). The company uses its members’ aggregate purchasing power to negotiate pricing discounts, improved quality and resiliency of products and improved contract terms with suppliers. Contracted suppliers pay the company administrative fees based on the net negotiated price and purchase volume of goods and services sold to its members under the contracts it has negotiated. The company also partners with other organizations, including regional GPOs, to extend its network base to their members.
The company’s contract portfolio is designed to offer its members a flexible solution consisted of multi-sourced supplier contracts, as well as pre-commitment and/or single-sourced contracts that offer higher discounts. The company’s multi-sourced contracts offer pricing tiers based on purchasing volume and/or commitment and multiple suppliers for many products and services. The company’s pre-commitment contracts require that a certain amount of its members commit in advance to a specified amount or percentage of purchasing volume before it enters into a contract with a particular supplier. The company’s single-source contracts are entered into with a specified supplier, and through this exclusive relationship, allow it to contract for products that meet the company’s members’ specifications. In the case of pre-commitment contracts, the company provides the particular supplier with a list of members that have pre-committed to a specified amount or percentage of purchasing volume and the supplier directly handles the tracking and monitoring of fulfillment of such purchasing volume. In the case of single and multi-sourced contracts, the company negotiates and executes the contracts with suppliers on behalf of its members and make such contracts available to its members to access. The utilization of such single and multi-sourced contracts is determined by each particular member with assistance from the company’s field force. Since there are no specific fulfillment requirements needed in the company’s single and multi-source contracts in order to obtain certain pricing levels, each particular member and supplier agree on the appropriate pricing tier based on expected purchasing volume with tracking and ongoing validation of such purchasing volume provided by the supplier. The flexibility provided by the company’s expansive contract portfolio allows it to effectively address the varying needs of its members and the significant number of factors that influence and dictate these needs, including overall size, service mix, and the degree of integration between hospitals in a healthcare system.
The company continually innovates its GPO programs and supply chain platforms while targeting multiple markets, including acute and continuum of care site settings. In addition to the company’s core base of more than 4,350 acute care healthcare providers, Premier’s continuum of care program, one of the largest in the United States, which covers over 80 classes of trade, had approximately 300,000 active members as of June 30, 2023. A number of these members in Premier’s continuum of care program are affiliated, owned, leased or managed by the company’s members.
Premier’s continuum of care program includes direct members, group affiliates and healthcare provider offices affiliated, owned, leased or managed by health systems. Key classes of trade include long-term care pharmacies, skilled nursing and assisted living facilities, home infusion providers, home health providers and surgery centers. Premier continuum of care members have access to most of the company’s GPO supplier contracts, including but not limited to, pharmaceuticals, medical and surgical supplies, facilities, food and nutritional products and other purchased services.
Premier’s continuum of care program provides business operations and technology to ensure members and other customers, including former non-healthcare members, are connected to agreements and receiving proper contracted pricing.
Supply Chain Co-Management: The company manages and co-manages the supply chain operations for contracted members to drive down costs through processes, including value analysis, product standardization and strategic resource allocation and improved operational efficiency.
Purchased Services Contracts: The company’s purchased services contracts business, which is separate from the purchased services under its national contract portfolio, includes Conductiv, Inc. (Conductiv) and Conductiv Contracts, LLC (Conductiv Contracts). Conductiv is a SaaS provider of technology solutions and expert services that enable hospitals and other organizations to analyze, benchmark and source purchased service contracts independent of any existing GPO affiliation. Combined with the company’s purchased services spend data and its performance improvement technology suite, it is able to be a single source provider for healthcare margin improvement. Conductiv Contracts is a regionally focused group purchasing organization independent of any existing GPO affiliation that exclusively focuses on purchased services contracting.
Direct Sourcing: The company’s direct sourcing business, SVS, LLC doing business as S2S Global (S2S Global), helps its members and other customers access a diverse product portfolio and helps provide transparency to manufacturing costs and competitive pricing. Through S2S Global, the company facilitates the development of product specifications with its members and other customers, source or contract manufacture the products to member specifications and sell products directly to its members, other customers or distributors. By engaging with the company’s members and other customers at the beginning of the sourcing process to define product specifications and then sourcing, or contract manufacturing, products to meet the exact needs of its members, it eliminates the need for unnecessary product features and specifications that may typically be included by suppliers and result in higher prices for its members without providing incremental value. Therefore, the company’s direct sourcing activities benefit its members and other customers by providing them with an expanding portfolio of medical products through more efficient means, and with greater cost transparency, than if such products were purchased from other third-party suppliers. The company markets its direct sourcing activities to its members primarily under the PREMIERPRO brand.
Supply Chain Resiliency Program: In partnership with its members, the company has created a program designed to promote domestic and geographically diverse manufacturing and ensure a robust and resilient supply chain for essential medical products. The program is intended to provide a means to invest in or partner with businesses that can supply shortage products, co-fund the development of affordable products that address specific market needs and create strategic sourcing contracts to ensure continuous supply for its members and customers.
The company’s Supply Chain Resiliency Program includes, but is not limited to, the following:
PRAM Holdings, LLC: The company formed PRAM Holdings, LLC (PRAM) in 2020 in partnership with member health systems to invest in Prestige Ameritech Ltd. (Prestige), a domestic manufacturer of masks, sterile intravenous solutions and other personal protective equipment (PPE), whereby its members obtain a direct domestic source to critical PPE.
DePre Holdings, LLC: The company formed DePre Holdings, LLC (DPH) in 2021 in partnership with member health systems to invest in DePre, LLC (DePre), a joint venture between DPH and DeRoyal Industries Inc., a global medical manufacturer, whereby its members obtain a direct source dedicated to the domestic production of isolation gowns.
ExPre Holdings, LLC: The company formed ExPre Holdings, LLC (ExPre) in 2022 in partnership with member health systems to invest in Exela Holdings, Inc. (Exela), a domestic manufacturer of proprietary and generic sterile injectable products, whereby its members obtain a direct source to certain critical pharmaceutical products.
Premco, LLC: The company formed Premco, LLC (Premco) in 2023 in partnership with member health systems to invest in Princo, LLC (Princo), a joint venture between Premco, Vario Labs LLC and Caretrust LLC, whereby its members obtain a direct source dedicated to the domestic production of incontinence pads.
SaaS Informatics Products: Members of the company’s GPO have access to certain SaaS informatics products related to the supply chain and have the ability to purchase additional elements.
Performance Groups: The company’s Performance Groups are highly committed purchasing programs, which enable members to benefit from coordinated purchasing decisions and maintain standardization across their facilities. The company’s Performance Groups include the ASCENDrive and the SURPASS Performance Groups.
ASCENDrive Performance Group: The company’s ASCENDrive Performance Group (ASCENDrive) has developed a process to aggregate purchasing data for its members, enabling such members to benefit from committed group purchases within the Performance Group. Through ASCENDrive, members receive group purchasing programs, tiers and prices specifically negotiated for them and knowledge sharing with other member participants. As of June 30, 2023, approximately 1,700 U.S. hospital members, which represent over 131,000 hospital beds, participated in ASCENDrive.
SURPASS Performance Group: The company’s SURPASS Performance Group (SURPASS) builds upon and complements ASCENDrive and drives even greater savings for members at a correspondingly higher level of commitment. SURPASS brings together its most committed members that are able to coordinate purchasing decisions, review utilization and achieve and maintain standardization across their facilities. SURPASS utilizes the company’s PACER (Partnership for the Advancement of Comparative Effectiveness Review) methodology, which brings together clinically led cohorts to make evidence-based decisions about physician and clinician preference items with the intention of materially reducing the total cost of care. As of June 30, 2023, a group of 33 members represented approximately 530 acute care sites and 11,000 continuum of care sites participate in SURPASS.
Performance Services segment
This segment consists of three sub-brands: PINC AI, Contigo Health and Remitra. Each sub-brand serves different markets but are all united in its vision to optimize provider performance and accelerate industry innovation for better, smarter healthcare. The company’s PINC AI platform enables it to better reflect its product offerings and strategy to expand and responsibly incorporate artificial intelligence (AI) across its portfolio of solutions. This platform further enables connectivity and scale between providers, the pharmaceutical, biotech, and medical device industry and payers, including large employers, to help lower the cost and improve the quality of care. The company houses one of the largest clinical, operational and financial datasets in the United States which enables actionable insight and real-world evidence needed to accelerate healthcare improvements. The company incorporates AI into several use cases, including prior authorization between payers and providers; clinical intelligence through the decision support process; and automating the invoicing and payables process. The company’s AI use cases are focused on helping key healthcare stakeholders improve the quality, efficiency and value of healthcare delivery. Using its data and scale, the company seeks to expand its AI capabilities, grow its overall portfolio of solutions and provide its members and customers with technologically advanced products so they can provide better, smarter healthcare.
PINC AI
With a broad provider network, advanced analytics, and the incorporation and desired expansion of AI-powered technology backed by the company’s large dataset, PINC AI has the ability to accelerate ingenuity in healthcare.
PINC AI helps optimize performance in three main areas – clinical intelligence, margin improvement and value-based care – using advanced analytics to identify improvement opportunities, consulting services for clinical and operational design and workflow solutions to hardwire sustainable change.
Clinical intelligence solutions help drive greater clinical effectiveness and efficiency across the care continuum by:
Surfacing analytics and peer benchmarking on hard-to-find, high-value quality improvement areas, helping providers improve care delivery;
Delivering real-time clinical surveillance to help providers drive faster, more informed decisions regarding patient safety, including ongoing infection prevention (like COVID-19), antimicrobial stewardship, and reduction of hospital acquired conditions;
Using AI-enabled clinical decision support integrated into the provider workflow to support evidence-based decisions by providers at the point of care, and improve prior authorization automation;
Operating the QUEST Collaborative, which works to develop quality, safety and cost metrics with a consistency and standardization. Participation in the QUEST Collaborative better prepares providers to deal with evolving and uncertain healthcare reform requirements and differentiate on care delivery in their markets; and
Providing life sciences services through PINC AI Applied Science for the development of research, real-world evidence and clinical trials innovation for medical device, diagnostic and pharmaceutical companies.
Margin improvement solutions help lower total costs and improve provider operating margins by:
Surfacing analytics and peer benchmarking on hard-to-find, supply savings and workforce management opportunities that lower costs without impacting quality;
Optimizing workforce management with integrated financial reporting and budgeting across the continuum of care;
Providing savings through an enterprise resource planning solution built specifically for healthcare;
Deploying consulting services to deliver clinically integrated, margin improvement transformation throughout a health system; and
Providing management services to insurance programs to assist the U.S. hospital and healthcare system members with liability and benefits insurance services, along with risk management services to improve their quality, patient safety and financial performance while lowering costs.
Value-based care solutions help health systems implement effective models of care to succeed in new, value-based payment arrangements by:
Surfacing analytics and peer benchmarking to help identify hard-to-find, population-based improvement opportunities necessary to take financial risk and succeed in value-based care;
Optimizing and managing the physician enterprise to rationalize medical group investment via revenue enhancement, cost reduction strategies and implementation of sustainable evidence-based practices; and
Participating in the Population Health Management, Bundled Payment and Physician Enterprise Collaboratives, for the opportunity to share value-based care and payment developmental strategies, programs and best practices.
The data yielded through PINC AI is de-identified and aggregated to be the nation’s leading comprehensive database, representing over 20 years of data from more than 1,000 hospitals spanning multiple therapeutic areas. A research team, including clinicians, epidemiologists, health economists, health services researchers, statisticians and other subject matter experts leverage the dataset to deliver real world evidence, in partnership with Life Science innovators. Studies, test methods, strategies and tools created can promote the adoption and integration of evidence-based practices to help improve outcomes and the quality and effectiveness of care.
Contigo Health
Contigo Health creates new ways for clinicians, health systems and employers to work together supporting a common goal for all stakeholders to help increase access to high-quality care, enhance employee engagement, control costs and get employees back to work and life faster. Contigo Health delivers comprehensive services for optimizing employee health benefits, including:
Contigo Health Sync Health Plan third-party administrative (TPA) empowers self-funded employers with a flexible approach to employee benefits to help improve access to quality care, achieve cost savings and improve health plan member satisfaction;
Contigo Health Centers of Excellence 360 delivers access to high-quality care by bringing together specialty medical and behavioral health programs for a bundled cost through a network of healthcare facilities, surgeons, physicians and leading-edge virtual providers; and
Contigo Health ConfigureNet Out-of-Network Wrap delivers an out-of-network wrap product to improve access to healthcare and reduce the cost of medical claims through pre-negotiated discounts with its network of 900,000 providers across the U.S. and Puerto Rico.
Remitra
Remitra provides health systems and suppliers cost management solutions with the company’s procure-to-pay technology designed to support greater efficiencies in the procurement process through automated purchasing and payment solutions.
Remitra’s Procure-to-Pay platform powers supplier and provider networks and uses optical character recognition to automate invoicing and payables. Remitra seeks to streamline financial processes, reduce errors and fraud, unlock cost and labor efficiencies and become a leading digital invoicing and payables platform for all of healthcare, agnostic of ERP, GPO or treasury partner.
Remitra’s Cash Flow Optimizer platform offers a financial solution for suppliers and providers, including a reduction in days sales outstanding, improving on-time payments, improved working capital and a potential reduction over time of allowance of credit losses associated with bad debt.
Remitra’s Managed Account Payable services offers a financial solution for acute and continuum of care members and other customers, including an extension in days payable outstanding, improving on-time payments for suppliers and improving working capital for the customer.
Both Remitra’s Cash Flow Optimizer platform and Managed Account Payable services offer financial solutions by leveraging Remitra’s Procure-to-Pay platform and providing opportunities for financial improvements for suppliers, members and other customers.
The Performance Services sub-brands support Premier’s long-term strategy to diversify revenue into adjacent markets, which the company defines as non-traditional markets penetrated by Premier’s businesses and brands. This includes PINC AI Clinical Decision Support serving providers and payers; PINC AI Applied Sciences serving biotech, pharmaceutical and medical device companies; Contigo Health that serves self-insured employers, including payviders; and Remitra that serves healthcare suppliers and providers.
Trademarks, Trade Names and Service Marks
The trademarks, trade names and service marks that the company either owns or licenses, such as but not limited to Acurity, ASCENDrive, Conductiv, ConfigureNet, Contigo Health, Essensa, Health Design Plus, Innovatix, InterSectta, KIINDO, PINC AI, Premier, PremierPro, ProvideGx, QUEST, Remitra, SURPASS, S2S Global and TheraDoc, which are protected under applicable intellectual property laws.
Government Regulation
To help ensure regulatory compliance with the Department of Health and Human Services (HHS) rules and regulations, the company’s members that report their costs to Medicare are required under the terms of the Premier Group Purchasing Policy to appropriately reflect all elements of value received in connection with its initial public offering (IPO), including under the various agreements entered into in connection therewith, on their cost reports.
The company’s business is also subject to numerous federal and state laws that forbid the submission or causing the submission of false or fraudulent information or the failure to disclose information in connection with the submission and payment of claims for reimbursement to Medicare, Medicaid or other governmental healthcare programs or private health plans.
The company’s self-funded health benefit plan and its healthcare provider members (provided that these members engage in HIPAA-defined standard electronic transactions with health plans, which will be all or the vast majority) are directly regulated by the Health Insurance Portability and Accountability Act of 1996 (HIPAA) as ‘covered entities’.
Competition
The company’s Supply Chain Services segment’s competitors primarily compete with its group purchasing, direct sourcing and supply chain co-management activities. The company’s group purchasing business competes with other large GPOs, such as HealthTrust Purchasing Group (a subsidiary of HCA Holdings, Inc.); Managed Health Care Associates, Inc.; and Vizient, Inc. In addition, the company competes against certain healthcare provider-owned GPOs and on-line retailers in this segment. The company’s direct sourcing business competes primarily with private label offerings and programs, product manufacturers, and distributors, such as Cardinal Health, Inc., McKesson Corporation, Medline Industries, Inc. and Owens & Minor, Inc. The company’s supply chain co-management business competes with organizations that provide supply chain outsourcing or embedded resources and supply chain transformation services, such as The Resource Group and CPS Solutions, LLC.
The company’s Performance Services segment’s competitors compete with its three sub-brands: PINC AI, Contigo Health and Remitra. The primary competitors of PINC AI range from smaller niche companies to large, well-financed and technologically sophisticated entities. The company’s primary competitors for PINC AI include information technology providers, such as Veradigm, Inc.; Epic Systems Corporation; Health Catalyst, Inc.; IBM Corporation; Infor, Inc.; and Oracle Corporation, and consulting and outsourcing firms, such as Deloitte & Touche LLP; Evolent Health, Inc.; Healthagen, LLC (a subsidiary of Aetna, Inc.); Huron Consulting, Inc.; Guidehouse Consulting, Inc.; Optum, Inc. (a subsidiary of UnitedHealth Group, Inc.); and Vizient, Inc. The primary competitors for Contigo Health include AmeriBen, Meritan Health, UMR, WebTPA and Benefit and Risk Management Services for the company’s third-party administrative services product; Carrum Health, Transcarent, Edison Healthcare, AccessHope and MSK Direct for its Centers of Excellence product; and First Health, MultiPlan, Zelis and other wrap network providers and major carriers (such as Aetna, United and Cigna) for its ConfigureNet product. The primary competitors for Remitra include Global Healthcare Exchange, LLC for the company’s digital invoicing product, Coupa Software Inc. and Taulia for its digital payables product, and tier one treasury banks (e.g., JPMorgan Chase and Co., Wells Fargo, Bank of America, etc.), as well as niche factoring companies for its financing solutions product.
History
Premier, Inc. was incorporated in Delaware in 2013.

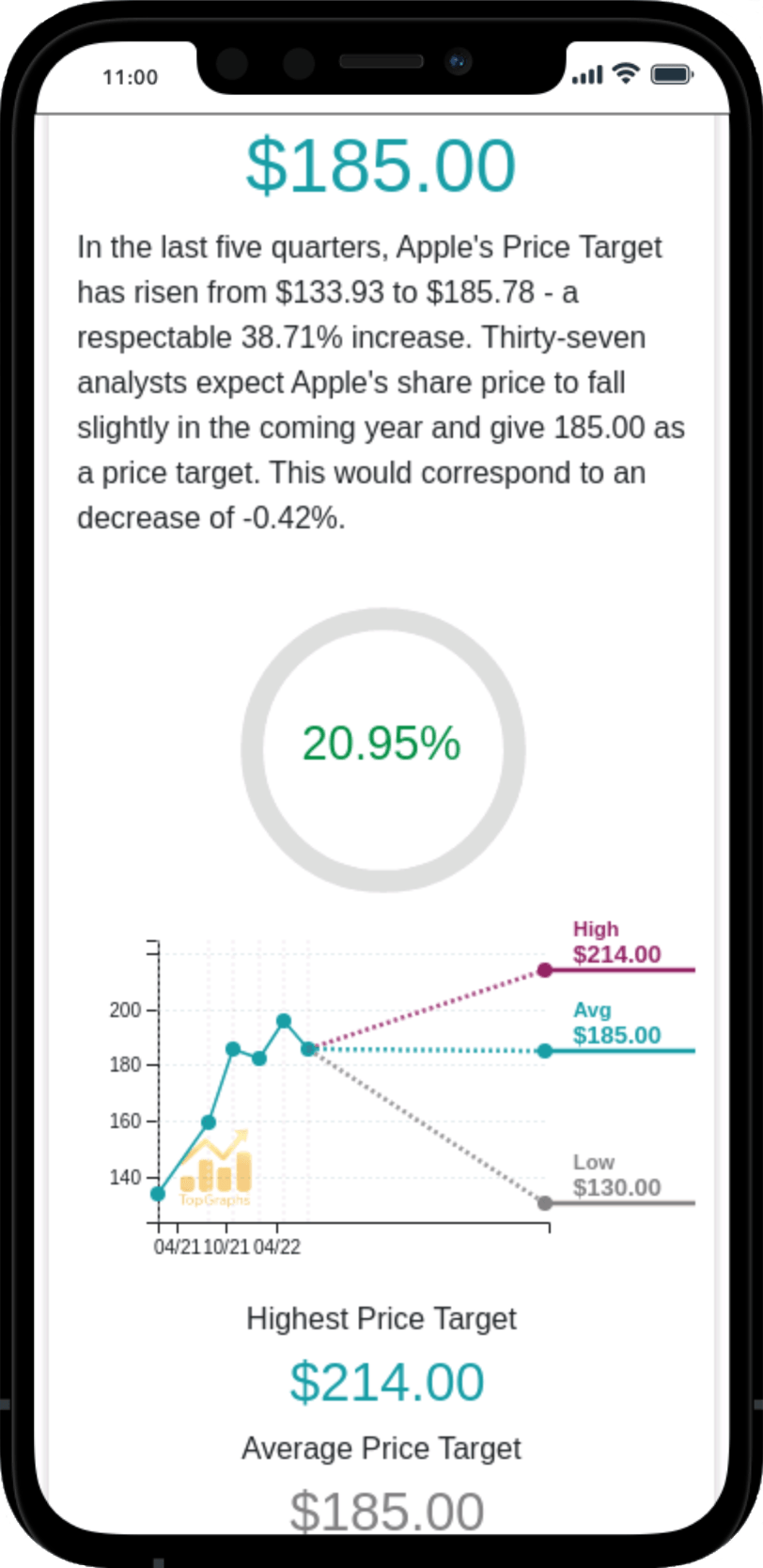
 Stock Value
Stock Value