About Performant Financial
Performant Financial Corporation provides technology-enabled audit, recovery, and analytics services in the United States with a focus in the healthcare industry.

The company works with healthcare payers through claims auditing and eligibility-based (also known as coordination-of-benefits or COB) services to identify improper payments. The company engages clients in both government and commercial markets. The company also has a call center which serves clients with multifaceted consumer engagement needs. The company’s clients typically operate in complex and highly regulated environments and contract for their payment integrity needs in order to reduce losses on improper healthcare payments.
The company has a leading position in its markets based on its technology-enabled services platform, long-standing client relationships, and the large volume of claims or funds it has audited and recovered for its clients. The company’s business platforms are adaptable to new markets and new processes and service offerings within its existing markets. The company continues to enhance its platforms through investments in new data and analytics capabilities, which will enable it to provide additional services related to the detection of fraud, waste and abuse. The company’s revenue model is generally success-based as it earns fees on the aggregate correct audits and/or amount of funds that it enables its clients to recover.
Markets
The company operates in markets characterized by strong growth, a complex regulatory environment and a significant amount of delinquent, defaulted or improperly paid assets.
Growth Strategy

The key elements of the company’s growth strategy are to expand its payment integrity services in the healthcare market; and pursue strategic alliances and acquisitions.
Platform
The company’s data management, analytics, and technology-enabled services platform is proprietary and based on over two decades of experience in auditing and recovering large amounts of funds on behalf of its clients across several markets. The components of the company’s platform include The company’s data management expertise, data analytics capabilities and technology-based workflow processes. The company’s platform integrates these components to allow it to achieve optimized outcomes for its clients in the form of increased efficiency and productivity and high efficacy rates. The company’s platform and workflow processes are also intuitive and easy to use for its healthcare claims specialists, which allow it to increase its employee retention and productivity.
The components of the company’s platform include the following:
Data Management Expertise
The company’s platform manages and stores large amounts of data throughout its workflow process. This data includes a combination of both publicly-available information, as well as proprietary and client specific data, the combination of which creates a robust input for claims review and selections. The company is able to integrate these sources efficiently and in real-time to reduce errors, reduce cycle time processing and, ultimately, improve audit finding and recovery rates. The strength of the company’s data management expertise augments its data analytics capabilities and provides its healthcare claims specialists with powerful workflow processes.
Data Analytics Capabilities
The company’s data analytics capabilities are designed to efficiently screen and allocate massive volumes of claims inventory. For example, the company analyzes millions of healthcare claims with customized payment integrity algorithms to find potential correlations between claims data and improper payments, which enhance its finding rates. The company utilizes its proprietary analytics tools across all of its markets and clients to continuously and rigorously test its workflow processes in real-time in order to drive greater process efficiency and improvement in recoupment rates.
Furthermore, the company’s data analytics capabilities will enable it to extend its potential product offerings within the healthcare market, permitting it to pursue significant new business opportunities.
Workflow Processes
Over many years, the company has developed and refined its workflow processes, which drive higher efficiency and productivity and reduce its reliance on labor-intensive methods relative to more traditional outsourcing models. The company’s technology supports its proprietary workflows to disaggregate otherwise complex processes into a series of simple, efficient and consistent steps that are easily configurable and applicable to different types of applications. These allow subject matter experts to quickly review analytical outputs and achieve targeted audit and recovery outcomes for the company’s clients.
Services
The company uses its technology-enabled services platform to provide services for the identification and recovery of improper payments, primarily in the healthcare market.
Healthcare
The company provides payment integrity services related to improper payments in the healthcare market, serving both government and commercial clients. Within the healthcare market, the company has strong and established relationships with multiple government agencies across its various product lines.
In October 2016, the company was awarded two RAC contracts by CMS. One of these RAC contracts, which was subsequently re-awarded to the company in 2021 for an eight-and-a-half year term, covers Parts A and B Medicare payments in Region 1. The second RAC contract involves post-payment review of DMEPOS and home health and hospice claims across the entire U.S. In November 2022, the company was awarded a third RAC contract by CMS which is for an eight-and-a-half year term and covers Parts A and B Medicare payments in Region 2.
Under its RAC contracts with CMS, the company utilizes its technology-enabled services platform to screen Medicare claims against several criteria, including coding procedures and medical necessity standards, to determine whether a claim should be further investigated for recoupment or adjustment by CMS. The company conducts automated and, where appropriate, detailed medical necessity reviews. The company interacts and communicates with healthcare providers and other administrative entities, and ultimately submit the claim to CMS for correction.
In October 2017, the company was awarded the national exclusive MSP contract by CMS. This contract was subsequently re-awarded to the company in December 2022. Under its MSP contract with CMS, the company is responsible for identifying and recovering payments in situations where Medicare should not be the primary payer of healthcare claims because a beneficiary has other forms of insurance coverage, such as through an employer group health plan or certain other insurance payers.
In January 2022, the company was awarded the indefinite delivery, indefinite quantity contract by the U.S. Department of Health and Human Services, Office of the Inspector General (HHS OIG), which has a base term of one year and four additional one-year options. Under this contract, the company provides medical review and consultative services associated with the oversight activities of the HHS OIG, primarily assessing services and claims for Medicare fee-for-service payments for Part A and Part B.
In the private healthcare market, the company has entered into numerous private insurance payer contracts and are pursuing additional opportunities to provide audit, recovery, and analytics services. The company utilizes its technology-enabled services platform to provide audit, recovery, and analytics services for private healthcare payers. The company’s experience from its contracts with CMS has helped establish its presence in the private healthcare market resulting in opportunities for it to provide audit and recovery services for several national and regional commercial health plans. The company’s audit and analytics capabilities have allowed it not only to expand its services with these initial private healthcare clients, but also gain entry into other related private healthcare opportunities.
Recovery
The company has historically worked in recovery markets, such as defaulted student loans, federal treasury and state tax receivables, and commercial recovery.
Customer Care / Outsourced Services
The company derives revenues from first party call center and other outsourced services. The company’s revenues for these services include contingency fees, fees based on dedicated headcount, and tasks completed on behalf of its clients.
Analytics Capabilities
For several years, the company has leveraged its data analytics tools to help filter, identify audit claims and recover delinquent and defaulted assets and improper payments as part of its core services platform. Through its data analytics capabilities, which the company refers to as Performant Insight, the company are able to review, aggregate, and synthesize very large volumes of structured and unstructured data, at high speeds, from the initial intake of disparate data sources to the warehousing of the data, to the analysis and reporting of the data.
Performant Insight provides numerous benefits for the company’s audit and recovery services platform. Performant Insight has not only enhanced its existing services under its contracts with CMS and other private healthcare contracts by analyzing significantly higher volumes of healthcare claims at faster rates and reducing its cycle time to review and assess healthcare claims, but it has also enabled the company to develop improved and more sophisticated business intelligence rules that can be applied to its audit processes. The company’s analytics capabilities will extend its potential markets, permitting it to pursue significant new business opportunities. The company has expanded the use of its data analytics capabilities in the healthcare sector to offer a variety of services from post and pre-payment audit of healthcare claims in both the public and private healthcare sector, to detection of fraud, waste and abuse of healthcare claims, to coordination of benefits and pharmacy fraud detection.
Clients
The company provides its services across a range of government and private clients.
CMS
The company’s relationship with CMS extends approximately fourteen years. Under its first RAC contract with CMS, which was initially awarded in 2008 and expired in 2016, the company was responsible for identifying and facilitating the recovery of improper Part A and Part B Medicare payments in the Northeast region of the United States.
In October 2016, the company was awarded two new RAC contracts with CMS. The company received the contract to audit improper payments for claims made under Medicare Parts A and B in Region 1, which consists of eleven states (Connecticut, Michigan, Indiana, Maine, Massachusetts, New Hampshire, New York, Ohio, Kentucky, Rhode Island and Vermont), and the contract for Region 5, which involves post-payment review of claims related to DMEPOS and home health and hospice across the U.S. The fees that the company receives for identifying improper payments from CMS under these contracts are entirely contingency-based, and the contingency-fee percentage depends on the methods of recovery, and, in some cases, the type of improper payment that the company identify. In March of 2021, the company was re-awarded the CMS Region 1 contract with a term of eight-and-a-half years.
Additionally, in November 2022, the company was awarded the RAC contract to audit improper payments for claims made under Medicare Parts A and B in Region 2, which consists of 14 states (Illinois, Minnesota, Wisconsin, Nebraska, Iowa, Kansas, Missouri, Colorado, New Mexico, Texas, Oklahoma, Arkansas, Louisiana, and Mississippi). The company’s RAC contract for Region 2 has a term of eight-and-a-half years.
In October 2017, the company was awarded the national exclusive MSP contract by CMS. Under this MSP contract, the company its responsible for coordination-of-benefits claims, which includes identifying and recovering payments in situations where Medicare should not be the primary payer of healthcare claims because a beneficiary has other forms of insurance coverage, such as through an employer group health plan or certain other payers. The company commenced operations on the MSP contract in 2018. The company was re-awarded this contract in December 2022, with an expected commencement in March 2023.
Private Healthcare
In the private healthcare market, the company utilizes its technology-enabled services platform to provide audit, recovery and analytical services for private healthcare payers. The company’s experience from its contracts with CMS has helped establish its presence in the private healthcare market by providing the company the opportunity to provide audit and recovery services for several national and regional commercial health plans.
Sales and Marketing
The company’s new business opportunities have historically been driven largely by referrals and natural extensions of its existing client relationships, as well as a targeted outreach by its sales team and senior management. The company’s sales cycles are often lengthy, and demand high levels of attention from its senior management. At any point in time, the company are typically focused on a limited number of potentially significant new business opportunities. As a result, to date, the company has operated with a small sales and marketing team of experienced individuals with responsibility for developing new sales working in concert with its executive staff.
Technology Operations
The company’s technology operations are Livermore, California, with primary and redundant datacenters located in Santa Clara, California and Fort Worth, Texas. The company has designed its infrastructure for scalability and redundancy, which allows the company to continue to operate in the event of an outage at any of its datacenters. The company maintain an information systems environment with dedicated information technology and security teams managing an advanced architecture focused on network security intrusion detection, data loss prevention and training of staff with 24x7 monitoring and security incident response capabilities. The company utilize encryption technologies certified to FIPS 140-2 to protect sensitive data on its systems, all data during transmission and all data on redundancy or backup solutions. The company also maintain a comprehensive enterprise-wide information security program certified by 3rd party auditors that is based on industry standards such as HITRUST, ARS 5.0,NIST 800-53, SOC 1 Type II and PCI/DSS.
Intellectual Property
As of December 31, 2022, the company had four trademarks registered with the U.S. Patent and Trademark office: Performant Financial Corporation, Performant Insight, and Premiere Credit.
Competition
The company’s competition in the private healthcare market includes the other RAC service providers, including Cotiviti, LLC and Cotiviti GOV Services, and a variety of healthcare consulting and healthcare information services companies.
Government Regulation
The nature of the company’s healthcare business and its legacy recovery business requires that the company adheres to a complex array of federal and state laws and regulations. These include, but are not limited to, the Health Insurance Portability and Accountability Act, or HIPAA; the Health Information Technology for Economic and Clinical Health Act, or HITECH; the False Claims Act, or FCA; the Anti-Kickback Statute, or AKS; the Exclusion Statute, the Privacy Act of 1974; the Fair Debt Collection Practices Act, or FDCPA; the Fair Credit Reporting Act, or FCRA; the rules and regulations established by the Consumer Financial Protection Bureau, or CFPB; and related state laws.
The company’s Medicare recovery business subjects it to compliance with HIPAA and various related state laws that contain substantial restrictions and requirements with respect to the use and disclosure of an individual’s protected health information.
The company is required to notify affected individuals and government authorities of data security breaches involving unsecured protected health information. The Department of Health and Human Services Office of Civil Rights enforces HIPAA privacy violations; CMS enforces HIPAA security violations; and the Department of Justice enforces criminal violations of HIPAA.
As a contractor to federal government agencies, the company is required to comply with the Privacy Act of 1974. Its compliance effort includes initial and ongoing training of employees and contractors in their obligations under the Privacy Act. In addition, the company has implemented and maintains physical, technical and administrative safeguards and processes intended to protect all personal data consistent with or exceeding the company’s obligations under the Privacy Act.
As a government contractor, the company has Authorization to Operate, or ATO, licenses for CMS Recovery Audit Contractor (RAC) Regions 1 & 5 and HHS Office of Inspector General (OIG). ATOs currently in process include CMS RAC Region 2 and CMS Medicare Secondary Payer (MSP).
The company maintains a comprehensive enterprise-wide information security program based on industry standards, such as ARS 5.0, NIST 800-53 and PCI/DSS. In addition, the company hold SSAE – SOC 1 Type II certification, which provides assurance to auditors of third parties that it maintains the necessary controls and procedures to effectively manage third party data. For its healthcare business, the company is HITRUST certified, which helps ensure that its policies, procedures, and implementation conform to HIPAA guidelines.
The company’s compliance efforts include written procedures for compliance with the FDCPA and related state laws, employee training and monitoring, auditing client calls, periodic review, testing and retraining of employees, and procedures for responding to client complaints.
In the ordinary course of business, the company is sued for alleged violations of the Telephone Consumer Protection Act and comparable state laws, although the amounts involved in the disposition or settlement of any such claims have not been significant.
The company is also subject to the Fair Credit Reporting Act, or FCRA, which regulates consumer credit reporting and which may impose liability on the company to the extent that the adverse credit information reported on a consumer to a credit bureau is false or inaccurate.
History
Performant Financial Corporation was founded in 1976. The company was incorporated in 2003.

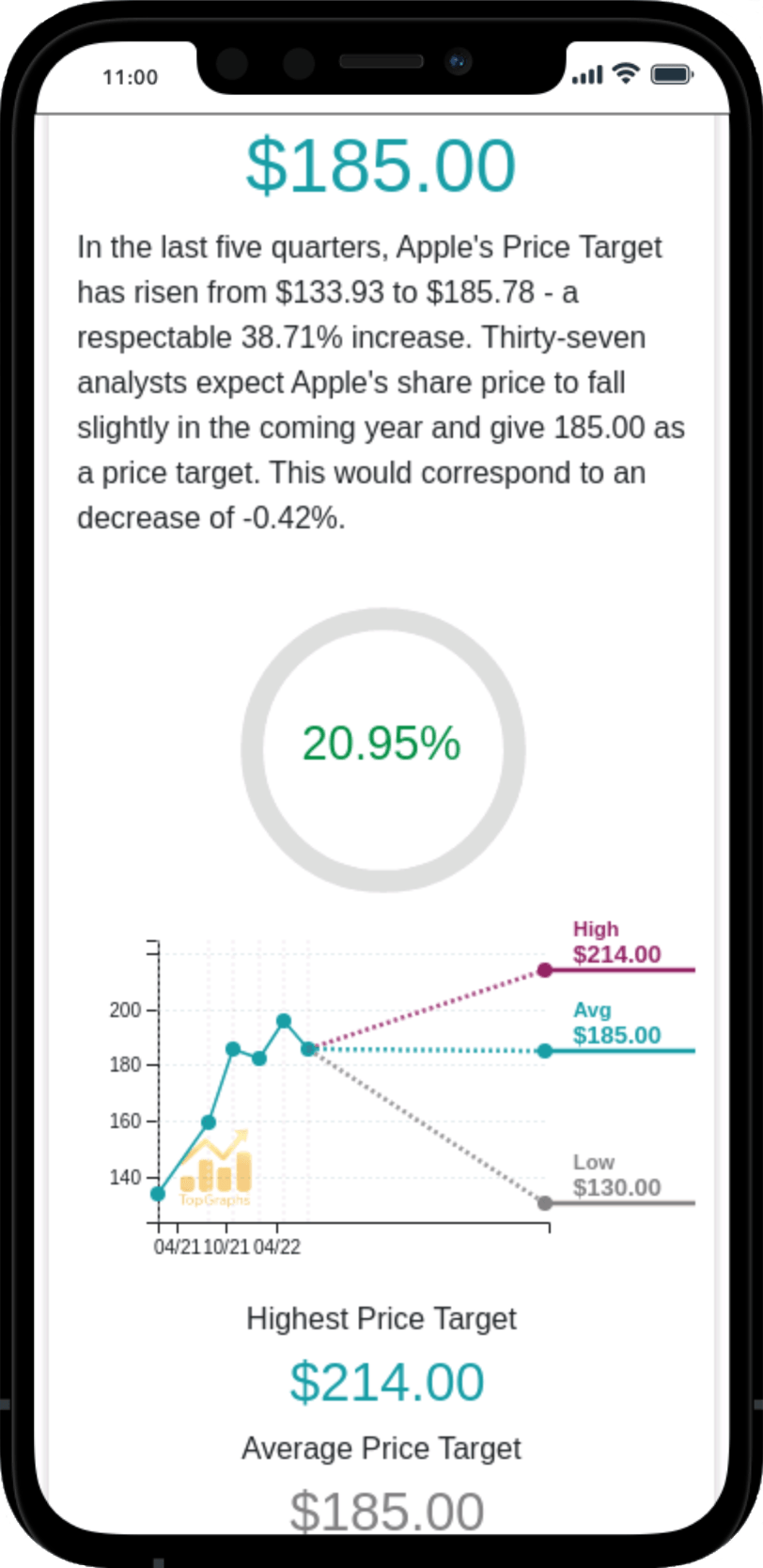
 Stock Value
Stock Value