About HealthEquity
HealthEquity, Inc. provides technology-enabled services that empower consumers to make healthcare saving and spending decisions. The company’s sole geographic market is the U.S.

The company uses its innovative technology to manage consumers' tax-advantaged health savings accounts (HSAs) and other consumer-directed benefits (CDBs) offered by employers, including flexible spending accounts and health reimbursement arrangements (FSAs and HRAs), and to administer Consolidated Omnibus Budget Reconciliation Act (COBRA), commuter and other benefits. As part of its services, the company provides consumers with healthcare bill evaluation and payment processing services, personalized benefit information, including information on treatment options and comparative pricing, access to remote and telemedicine benefits, the ability to earn wellness incentives, and investment advice to grow their tax-advantaged healthcare savings.
The core of the company’s offerings is the HSA, a financial account through which consumers spend and save long-term for healthcare expenses on a tax-advantaged basis. As of January 31, 2023, the company administered 8.0 million HSAs. The company refers to the aggregate number of HSAs and other CDBs that it administers as Total Accounts, of which it had 14.9 million as of January 31, 2023.
The company reaches consumers primarily through relationships with their employers, which it calls Clients. The company reaches Clients primarily through relationships with benefits brokers and advisors, integrated partnerships with a network of health plans, benefits administrators, benefits brokers and consultants, and retirement plan recordkeepers, which it calls Network Partners, and a sales force that calls on Clients directly. As of January 31, 2023, the company’s platforms were integrated with more than 200 Network Partners, and it serves more than 120,000 Clients.
The company earns revenue primarily from three sources: service, custodial, and interchange. The company earns service revenue mainly from fees paid by its Network Partners, Clients, and members for the administration services it provides in connection with the HSAs and other CDBs it offers. The company earns custodial revenue mainly from HSA Assets held at its members’ direction in federally insured cash deposits, insurance contracts or mutual funds, and from investment of Client-held funds, which are deposits remitted by Clients and held by it on their behalf to pre-fund and facilitate administration of CDBs. The company earns interchange revenue mainly from fees paid by merchants on payments that its members make using its physical payment cards and on its virtual payment system.
In March 2022, the company acquired the Health Savings Administrators, L.L.C. (HealthSavings) HSA portfolio.

The company’s solution is built on a business-to-business-to-consumer, or B2B2C, channel strategy, whereby it works with Network Partners and Clients to reach consumers in addition to marketing its services to these potential members directly. Reaching the consumer is critical in order for the company to increase the number of its HSA members. Health plan Network Partners have been, and continues to be, a key channel through which it gains access to clients and members.
The company works directly with its Network Partners and Clients to reach the consumer in various ways. The company’s health plan and administrator partners collectively employ thousands of sales representatives and account managers who promote both the health plan and administrator partner’s health insurance products, such as HDHPs, and its HSAs. The company’s Clients collectively employ thousands of human resources professionals who are tasked with explaining the benefits of its HSAs to their employees. The company’s sales and account management teams work with and train the sales representatives and account management teams of its Network Partners and the human resource professionals of its Clients on the benefits of enrolling in, contributing to, and saving and spending through its HSAs, and its Network Partners and Clients then convey these benefits to prospective members. As a result of this collaboration, the company develops relationships with each member who enrolls in an HSA with it. This personalized engagement with the company’s members constitutes its B2B2C channel strategy.
The company’s members utilize its technology platforms in a number of ways and in varying frequencies. For example, the company’s members utilize its HSA platform to evaluate and pay healthcare bills through the member portal, which allows members to pay their healthcare providers, receive reimbursements and learn of savings opportunities for prescription drugs. Members also utilize the platform’s mobile app to view and pay claims on-the-go, including uploading medical and insurance documentation to the platform with their mobile phone cameras.
The company’s solution was designed specifically to serve the needs of healthcare consumers, health plans and employers. The company provides with a solution that encompass all of the core functionality of healthcare saving and spending in integrated, secure, and compliant systems, including custodial administration of individual savings and investment accounts, card and electronic funds transaction processing, benefits enrollment and eligibility, electronic and paper medical claims processing, medical bill presentment, tax-advantaged reimbursement account and health incentive administration, HSA trust administration, online investment advice, and sophisticated analytics.
The company’s technology solution allows it to integrate data from disparate sources, which enables it to seamlessly incorporate personal health information, clinical insight, and individually tailored strategies into the consumer experience. The company has more than 20,000 distinct integrations with health plans, pharmacy benefit managers, employers, and other benefits provider systems. Many of the company’s partners’ systems rely on custom data models, non-standard formats, complex business rules, and security protocols that are difficult or expensive to change.
The company’s flexible technology solution enables it to create a unique solution for each of its Network Partners. For example, a HealthEquity team member can readily configure product attributes, including integration with a partner’s chosen healthcare price transparency or wellness tools, single sign on, sales and broker support sites, branding, member communication, custom fulfillment and payment card, savings options and interest rates, fees, and mutual fund investment choices.
Strategy
The company has historically acquired HSA portfolios and businesses that strengthen its business. The company expects to continue this growth strategy and regularly evaluate opportunities. The company has developed an internal capability to source, evaluate, and integrate acquisitions that have created value for stockholders.
Products and Services
Health Savings Accounts: The Medicare Modernization Act of 2003 created HSAs, a tax-exempt trust or custodial account managed by a custodian that is a bank, an insurance company, or a non-bank custodian specifically authorized by the Internal Revenue Service, or IRS, as meeting certain ownership, capitalization, expertise, and governance requirements. The company is an IRS-approved non-bank custodian of its members' HSAs, designated to serve as both a passive and non-passive non-bank custodian of HSAs.
Investment Platform and Advisory Services: The company offers a mutual fund investment platform and access to an online-only automated investment advisory service to all of its members whose account balances exceed a stated threshold. These services are entirely elective to the member. The advisory service is delivered through a web-based tool, Advisor, which is offered and managed by HealthEquity Advisors, LLC, the company’s SEC-registered investment adviser subsidiary. HealthEquity Advisors, LLC provides investment advice to its clients exclusively through the Advisor tool on an interactive website. Members who utilize the company’s mutual fund investment platform or subscribe for Advisor services pay asset-based fees, which include the cost of the advisory service and all other expenses associated with transactions made through these online tools.
Advisor provides investment education guidance and management, including maintaining HSA cash (liquidity) in amounts directed by the member, targeting risk appropriate portfolio diversification, and mutual fund selection.
The company offers investors access to three levels of service:
Self-Driven: For members who do not subscribe for Advisor, the company provides a mutual fund investment platform to invest HSA balances. Neither the company nor Advisor provides advice to members in respect of investments among funds on the platform;
GPS powered by HealthEquity Advisors, LLC: Advisor provides guidance and advice, but the member makes the final investment decisions and implements portfolio allocation and investment advice through the HealthEquity platform; and
AutoPilot powered by HealthEquity Advisors, LLC: Advisor manages the account and implements portfolio allocation and investment advice automatically for the member.
Regardless of the level of service selected, members are responsible for their proportionate share of fees and expenses payable by the underlying mutual funds and other investment vehicles in which they invest.
Healthcare flexible spending accounts. Healthcare FSAs are employer-sponsored CDBs that enable employees to set aside pre-tax dollars to pay for eligible healthcare expenses that are not generally covered by insurance, such as co-pays, deductibles and over-the-counter medical products, as well as vision expenses, orthodontia, and medical devices. Healthcare FSAs can be customized by employers so they have the freedom to determine what eligible expenses may be reimbursed under these arrangements. The company’s employer Clients also realize payroll tax (i.e., FICA and Medicare) savings on the pre-tax contributions made by their employees.
Dependent Care Flexible Spending Accounts: The company also administers FSA programs for dependent care plans. These plans allow employees to set aside pre-tax dollars to pay for eligible dependent care expenses, which typically include child care or day care expenses but may also include expenses incurred from adult and elder care.
HealthEquity administers the United States Office of Personnel Management's (OPM) Federal Flexible Spending Account Program (FSAFEDS). This relationship provides eligible federal government employees access to its advanced technology platforms and premium service capabilities.
Health Reimbursement Arrangements: Under HRAs, employers provide their employees with a specified amount of reimbursement funds that are available to help employees defray their out-of-pocket healthcare expenses, such as deductibles, co-insurance and co-payments. HRAs may only be funded by employers and there is no limitation on how much employers may contribute; however, similar to other CDBs that are funded with pre-tax dollars, employers are required to establish the programs in such a way as to prevent discrimination in favor of highly compensated employees. HRAs must either be considered an excepted benefit (for example, a dental-only HRA or a vision-only HRA), a retiree HRA or be integrated with another group health plan. HRAs can be customized by employers so employers have the freedom to determine what expenses are eligible for reimbursement under these arrangements. At the end of the plan year, employers have the option to allow all or a portion of the unused funds to roll over and accumulate year-to-year if not spent. All amounts paid by employers into HRAs are deductible for tax purposes by the employer and tax-free to the employee.
COBRA: The company offers COBRA continuation services to employer clients to meet the employer’s obligation to make available continuation of coverage for participants who are no longer eligible for the employer’s COBRA covered benefits, which include medical, dental, vision, HRAs and certain healthcare FSAs. COBRA requires employers to make health coverage available for qualified beneficiaries for a period of up to 36 months post-termination. As part of its COBRA program, the company offers a direct billing service where former employee participants pay it directly as opposed to their employers for coverage they elect to continue. The company handles the accounting and customer services for such terminated employees, as well as interfacing with the carrier regarding the employees’ eligibility for participation in the COBRA program.
Commuter Programs: The company administers pre-tax commuter benefit programs. Employers are permitted to provide employees with commuter benefits including qualified transit (which includes vanpooling) and parking. The maximum monthly federal (and sometimes state) tax free exclusion is indexed for inflation.
The company’s Luum technology platform provides employers with various commuter services, including access to real-time commute data, to help them design and implement flexible return-to-office and hybrid-workplace strategies and benefits.
Technology
Technology Platforms: The company provides multiple cloud-based platforms, accessed by its members online via a desktop or mobile device, through which individuals can make health saving and spending decisions, pay healthcare bills, compare treatment options and prices, receive personalized benefit and clinical information, earn wellness incentives, grow their savings and make investment choices. The platforms provide users with access to services the company provides, as well as services provided by third parties selected by it or by its Network Partners. The company’s delivery model for these platforms eliminates the need for its Clients to install and maintain hardware and software in order to support HSA and other CDB programs and enables it to rapidly implement product enhancements across its entire user base.
Among other features, the company’s HSA platform includes the capability to present to users medical bills upon adjudication by a health plan, including details, such as the amount paid by insurance, specific nature of the medical service provided, and diagnostic code. Users of its HSA platform can pay these bills from an account of its or from any bank account, online, via a mobile device, or using its payment card. All users of its HSA platform gain access to its healthcare consumer specialists, available every hour of every day, via a toll-free telephone number or email. The company’s specialists can assist users with such tasks as optimizing the use of tax-advantaged accounts to reduce medical spending or selecting from among medical plans offered by an employer or health plan.
The company acquired an additional technology platform as part of the Luum Acquisition, which provides Clients with various commuter services, including access to real-time commute data, to help Clients design and implement flexible return-to-office and hybrid-workplace strategies and benefits.
As of January 31, 2023, the company had substantially completed its efforts to phase out certain technology platforms that it acquired in the acquisition of its wholly owned subsidiary, WageWorks, Inc. (the WageWorks Acquisition), and migrate the associated clients to one of its other technology platforms. The company is working to phase out a technology platform that it acquired in the Further Acquisition, which requires it to migrate the associated clients to one of its other technology platforms.
Cloud-Based Solution: The company’s proprietary technology is deployed as a cloud-based solution that is accessible to customers online and through its mobile app. The company utilizes a multi-tenant architecture that allows changes made for one Network Partner to be extended to all others. This architecture provides operating leverage by reducing costs and improving efficiencies, enabling it to maximize the utilization of its infrastructure capacity with a reduction in required maintenance.
The company’s solution is delivered via cloud-based services and hosted in third-party data centers or on a virtual private cloud with an ability to scale on demand. This allows the company to quickly support its projected growth. The company utilizes regional cloud failover and multiple redundant third-party data centers to ensure continuous access and data availability. The data centers are purpose-built facilities for hosting mission critical systems with multiple built-in redundancy layers to minimize service disruptions and meet industry-standard measures.
Data Security and Protection: Due to the sensitive nature of the company’s customers’ data that it holds, it has heightened focus on data security and protection. The company maintains administrative, technical, and physical safeguards designed to protect confidential data. The company’s Risk and Security team identifies security risks by working with state and federal law enforcement, security information-sharing organizations, and 24/7 system surveillance through internal and external detection and response teams.
In the event a security risk is detected, or a breach occurs, the company is prepared with appropriate response protocols based on National Institute of Standards & Technology (NIST) guidelines. The company’s Security Incident Response Plan defines roles and responsibilities, incident severity levels, key contacts, post-incident steps, and guidelines for testing. The company’s procedures cover response steps for phishing attacks, ransomware, data breaches, and major vulnerabilities. Lastly, the company has an organic threat model that evaluates its security controls to help protect against attacker tactics, techniques, and procedures.
Competition
The company’s direct competitors include healthcare service companies, such as UnitedHealth Group's Optum, Webster Bank, and well-known retail investment companies, such as Fidelity Investments.
Government Regulation
The company’s business is subject to extensive, complex, and rapidly changing federal and state laws and regulations.
IRS Regulations: The company is subject to applicable IRS regulations, which lay the foundation for tax savings and eligible expenses under the HSAs, HRAs, and FSAs it administers The company is subject to conflict of interest and other prohibited transaction rules that are enforced through excise taxes under the Internal Revenue Code.
In February 2006, the company received designation by the U.S. Department of Treasury to act as a passive non-bank custodian, which allows it to hold custodial assets for individual account holders. In July 2017, the company received designation by the U.S. Department of Treasury to act as both a passive and non-passive non-bank custodian, which allows it to hold custodial assets for individual account holders and use discretion to direct investment of such assets held.
Privacy and Data Security Regulations: In the provision of HSA custodial services and directed TPA services for FSAs and HRAs, the company is subject to the Financial Services Modernization Act of 1999 (Gramm-Leach-Bliley Act or GLBA), the Health Insurance Portability and Accountability Act of 1996 (HIPAA, as amended by the Health Information Technology for Economic and Clinical Health Act), and similar state laws.
Because part of the company’s business is the administration of financial products, such as HSAs, the company is required under the Consumer Financial Protection Bureau’s financial privacy rule under GLBA to send a notice of privacy practices to account holders and to comply with restrictions on the disclosure of nonpublic personal information to non-affiliated third parties. The company is required under GLBA to establish reasonable administrative, technical, and physical safeguards to protect the security, confidentiality, and integrity of nonpublic personal information pursuant to the Federal Trade Commission’s safeguards rule.
The two rules that most significantly affect the company’s business are the Standards for Privacy of Individually Identifiable Health Information, or the Privacy Rule; and the Security Standards for the Protection of Electronic Protected Health Information, or the Security Rule. The Privacy Rule restricts the use and disclosure of protected health information, and requires the company to safeguard that information and provide certain rights to individuals with respect to that information.
ERISA: The company’s private-sector clients’ FSAs, HRAs, COBRA continuation insurance, and other account-based retirement plans are covered by the Employee Retirement Income Security Act of 1974, as amended, or ERISA, which governs employee benefits plans.
Department of Labor: The Department of Labor, or the DOL, regulates plans that are subject to ERISA, including health FSAs, HRAs, and 401(k) and other retirement plans, as well as COBRA administration.
Investment Advisers Act of 1940: The company’s subsidiary HealthEquity Advisors, LLC is an SEC-registered investment adviser that provides web-only automated investment advisory services to members. As an SEC-registered investment adviser, it must comply with the requirements of the Investment Advisers Act of 1940, or the Advisers Act, and related Securities and Exchange Commission, or SEC, regulations and is subject to periodic inspections by the SEC staff.
History
HealthEquity, Inc. was founded in 2002. The company was incorporated as a Delaware corporation in 2002.

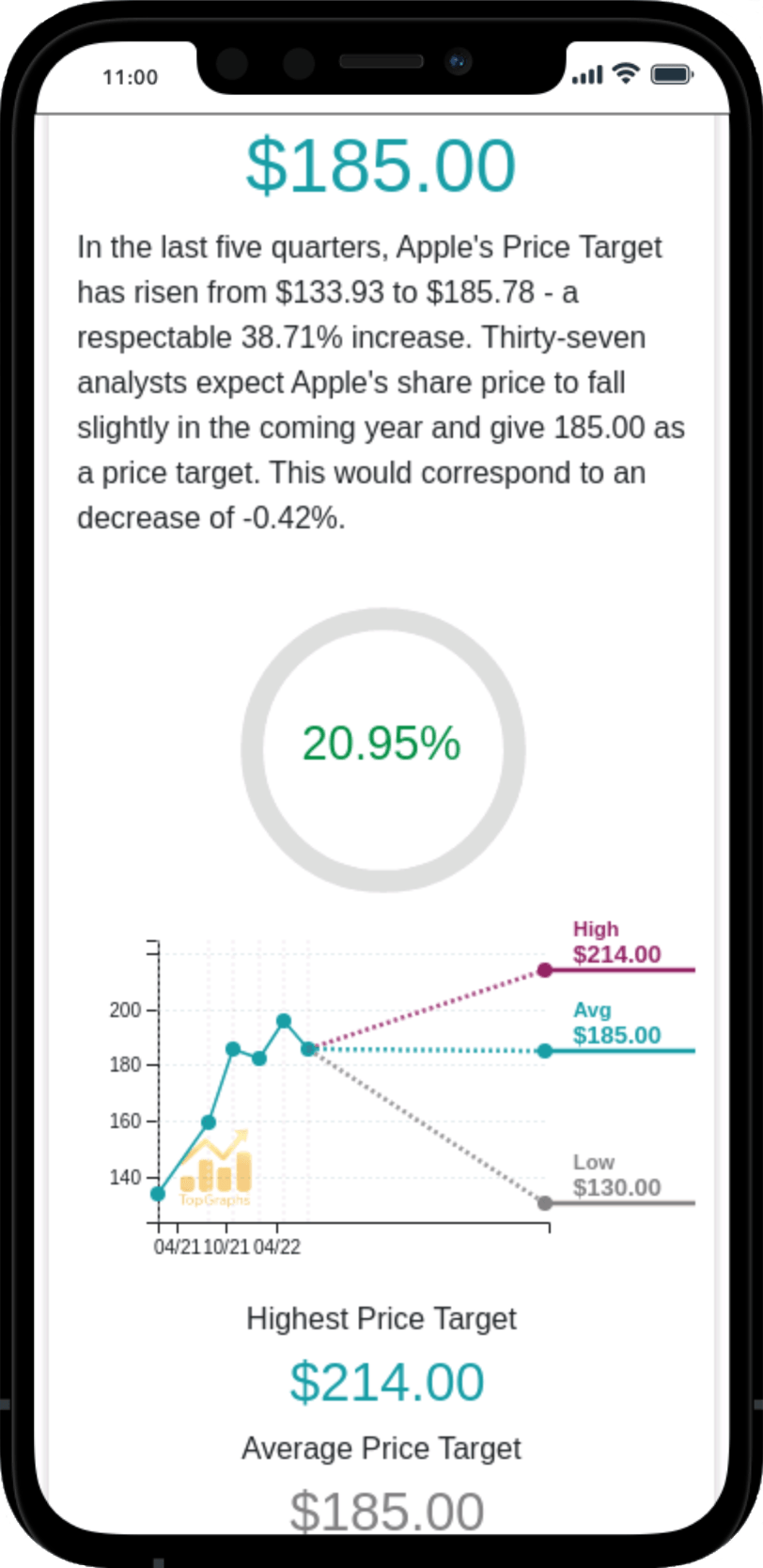
 Stock Value
Stock Value