About Evolent Health
Evolent Health, Inc. (Evolent), through its subsidiaries, is a market leader in connecting care for people with complex conditions like cancer, cardiovascular disease, and musculoskeletal diagnoses.

The company works on behalf of health plans and other risk-bearing entities and payers (its customers) to support physicians and other healthcare providers (its users) in providing high quality evidence-based care to their patients.
In October 2018, the company acquired New Century Health, a national population health leader in managing specialty care for Medicare, commercial and Medicaid members under performance-based arrangements, focused primarily on oncology and cardiovascular care, initiating Evolent's current primary strategy to pursue solutions for managing high prevalence, complex specialty care. To add to the company's capabilities, in October 2021, the company acquired Vital Decisions, a leading provider of technology-enabled advance care planning services. In August 2022, the company acquired IPG, a leader in providing surgical management solutions for musculoskeletal conditions. In January 2023, the company acquired NIA, a specialty benefit management organization that focuses on managing cost and quality in the areas of radiology, musculoskeletal, physical medicine and genetics.
The company provides a broad spectrum of specialty care management services in oncology, cardiology, musculoskeletal markets and holistic total cost of care management along with an integrated platform for health plan administration and value-based business infrastructure under one go to market package.
Solutions
The company has three primary solutions: (i) specialty care management services, (ii) total cost of care management and (iii) administrative services. From time to time, the company packages its solutions under various go-to-market brand names to create product differentiation. The company's partners may engage the company to provide one, or multiple types of solutions, depending on their specific needs.

Specialty Care Management Services Solution
The foundation for the company's specialty care management services solution was the company's acquisition in 2018 of New Century Health, a national leader in managing specialty care for Medicare members under performance-based and technology and services arrangements. Since then, the company has continued to invest in the solution to broaden, deepen, and scale its capabilities. The company focuses on the oncology, cardiology, and musculoskeletal markets, supported by diagnostics like radiology and genetic testing, with the objective of helping providers and payers deliver higher quality, more affordable care. In addition, the company provides comprehensive quality management for oncology and cardiology patients from diagnosis through advance care planning services as well as identifying high quality, lowest cost of care for outpatient orthopedic surgeries.
The company provides a differentiated approach by (i) assembling networks of high-performance providers, (ii) designing evidence-based clinical pathways and (iii) deploying proprietary specialty care management technology.
Assembling high-performance provider networks
The company develops high-performance provider networks with tools, capabilities and incentives to align and support physicians and other healthcare providers. The company develops and manages comprehensive specialty networks, provide physician engagement and support and identify provider financial incentive alignment.
Designing evidence-based clinical pathways
The company designs high-quality evidence-based clinical pathways to drive provider behavior towards improved quality of care at a lower cost.
The company's clinical pathways are based on national guidelines with independent scientific advisory boards, in-house clinical expertise with original publications and presentations at national congress. The company employs a collaborative review process that is not based on denials, which includes customized clinical review based on tier 1-5 drugs and proactive monitoring response to therapy. The company employs quality metrics and clinical benchmarking to continually improve the company's pathways.
Deploying proprietary specialty care management technology
The company's legacy New Century Health business leverages a custom specialty care management workflow platform, CareProTM, to provide clinical decision support and manage providers to high-quality care, while aiming to achieve significant cost savings. The company's technology consists of a clinical decision support portal that provides oversight of individual treatment plans for pathway adherence. The company's platform integrates clinical analytics and protocols, pharmacy management, physician engagement, network management and claims payment to drive improved outcomes for partners.
Total Cost of Care Management Solution
The company's total cost of care management solution enables providers to manage populations they may be accountable for under value-based contracts with payers or ACO contracts with CMS. This solution seeks to reduce the total cost of care for a given population by identifying and managing high-cost patients with targeted interventions managed and coordinated through primary care physicians. The company uses different go-to-market brand names for various solution packages, depending on the markets the company seeks to address. These go-to-market brand names include: (i) Value Based Services, wherein the company support primarily health systems in their value-based operations and (ii) Evolent Care Partners, wherein the company offers physicians the opportunity to join Evolent's proprietary payer contracting vehicles, scaled risk pools, and operating model.
The company refers to the offerings within this solution increasingly as 'Complex Care.' Core elements of this solution include: (i) population health performance, which supports the delivery of patient-centric cost-effective care and (ii) delivery network alignment, comprising the development of high performance delivery networks. The company integrates change management processes and ongoing physician-led transformation into all value-based services to build engagement, integration and alignment within the company's partners to successfully deliver value-based care and sustain performance. The company has standardized the processes described below and are able to leverage the company's expertise across the company's partner base. Through the technological and clinical integration, the company achieves, its solutions are delivered as engrained components of the company's partners' core operations rather than as add-on solutions.
Administrative Services
The company's administrative services solution includes its integrated value-based care platform designed to help the company's customers manage and administer patient health in a more cost-effective manner. The company has invested in its primary platform to facilitate value-based care business models for health plans called Identifi along with the company's clinical solutions to offer an integrated value-based care platform.
The company's comprehensive health plan administration services help regional and national payers and providers assemble the infrastructure required to operate, manage and capitalize on a variety of financial and administrative management services, such as health plan services, risk management, analytics and reporting and leadership and management. Historically, the economic model of this solution is primarily fee-based with defined service-level agreements around key operating metrics. The administrative services provided by the company include:
Health plan services: Health plan services is a comprehensive suite of services, including third-party administration, enrollment and billing support, medical and utilization management, third-party payment and program integrity support and provider network contracting services. Other health plan related services include sales and marketing, product development, actuarial, and regulatory and compliance.
Pharmacy benefit management: The company's team of professionals support the prescription drug component of providers' plan offerings and bring national buying power and dedicated resources that are tightly integrated with the care delivery model. Differentiated from what the company considers to be traditional PBMs, the company's solution is integrated into patient care and engages population health levers including generic utilization, provider management, and utilization management to reduce pharmacy costs.
Risk management: The company's risk management services provide the capabilities needed to successfully manage risk for payers, including analysis, data and operational integration with payer processes, and ongoing performance management.
Analytics and reporting: The company's analytics and reporting services provide the ongoing and ad hoc analytic teams and reports required to measure, inform and improve performance, including population health analytics, market analytics, network evaluation, staffing models, physician effectiveness, clinical delivery optimization and patient engagement.
Leadership and management: The company's local and national talent assist its partners in effectively managing the performance of their value-based operations.
Identifi is the company's proprietary technology system that aggregates and analyzes data, manages care workflows and engages patients. Identifi links the company's processes with those of its partners and other third parties to create a connected clinical delivery ecosystem, stratify patient populations, standardize clinical workflows and enable high-quality, cost-effective care. The configurable nature and broad capabilities of Identifi help enhance the benefits the company's partners receive from its services and increase the effectiveness of the company's partners' existing technology architecture. In addition, Identifi provides support and value to the company's specialty care management services and total cost of care management customers in a limited fashion. Highlights of the capabilities of Identifi include the following:
Data and integration services: Data from disparate sources, such as EMRs, and lab and pharmacy data, is collected, assembled, integrated and maintained to provide health care professionals with a holistic view of the patient.
Clinical and business content: Clinical and business content is applied to the integrated data to create actionable information to optimize clinical and financial performance.
EMR integration: Data and clinical insights from Identifi are fed back into partner EMRs to improve both provider and patient satisfaction, create workflow efficiencies, promote clinical documentation and coding and provide clinical support at the point-of-care.
Applications: A suite of cloud-based applications manages the clinical, financial and operational aspects of the value-based model. The company's applications scale with the clinical, financial and administrative needs of the company's provider partners. As additional capabilities are required by the company's partners, they are often deployed as applications through Identifi.
Growth Opportunities
The company's strategies include multiple avenues for growth with the company's existing, embedded partner base; ability to capture additional value through delivering clinical results; expanding offerings to meet evolving market needs; and selectively pursuing strategic acquisitions, investments and divestitures.
Sales and Marketing
The company markets and sells its services to payers and providers throughout the United States. The company's sales team works closely with its leadership team and subject matter experts to foster long-term relationships with the company's partners' leadership and board of directors given the nature of the company's partnerships. The company's dedicated business development team works closely with its partners to identify additional service opportunities on a continuous basis.
Government Regulation
The company is subject to regulation by both CMS and state agencies with respect to certain services the company provides relating to Medicaid and Medicare programs.
The company is subject to various federal, state and local laws and rules regarding the use, security and disclosure of protected health information, personal information, and other categories of confidential or legally protected data that the company handles. Such laws and rules include, without limitation, HIPAA, the Federal Trade Commission Act, the Gramm-Leach-Bliley Financial Modernization Act of 1999 (Gramm-Leach-Bliley Act), and state privacy and security laws such as the California Privacy Rights Act. Privacy and security laws and regulations often change due to new or amended legislation, regulations or administrative interpretation. A variety of state and federal regulators enforce these laws, including but not limited to the U.S. Department of Health and Human Services, the Federal Trade Commission, state attorneys general and other state regulators.
By processing data on behalf of the company's partners, the company is subject to specific compliance obligations under privacy and data security-related laws, including HIPAA, the HITECH Act and related state laws.
Intellectual Property
The company's continued growth and success depend, in part, on its ability to protect the company's intellectual property and proprietary technology, including the company's Identifi software and CarePro platform.
History
Evolent Health, Inc. was founded in 2011. The company was incorporated as a Delaware corporation in 2014.

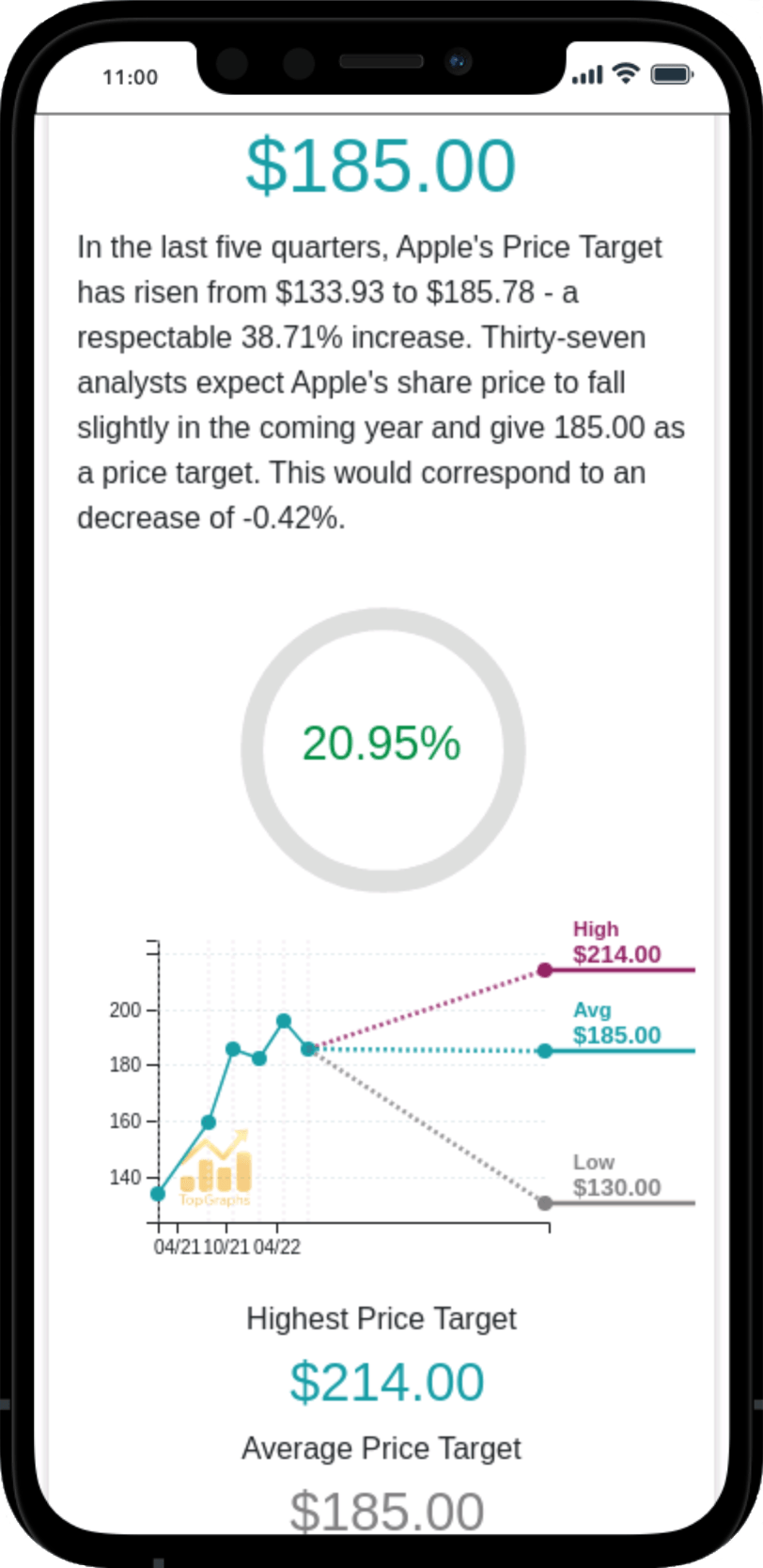
 Stock Value
Stock Value