About Employers Holdings
Employers Holdings, Inc. and its subsidiaries (EHI) operate as a specialty provider of workers' compensation insurance and services focused on small and select businesses engaged in low-to-medium hazard industries.

The company operates throughout the United States (U.S.), with the exception of four states that are served exclusively by their state funds. The company offers insurance through Employers Insurance Company of Nevada (EICN), Employers Compensation Insurance Company (ECIC), Employers Preferred Insurance Company (EPIC), Employers Assurance Company (EAC), and Cerity Insurance Company (CIC).
The company provides workers' compensation insurance throughout most of the United States, with a concentration in California, where 45% of the company’s in-force premiums are generated. The company markets and sells many of its insurance products through non-exclusive insurance agents and brokers.
Business Strategy
The company’s overall strategy is to pursue profitable growth opportunities across workers' compensation insurance market cycles, maximize the company’s investment returns within the constraints of prudent portfolio management, and deliver value to the company’s shareholders while being conscious of environmental, social and governance (ESG) concerns.
The company pursues profitable growth opportunities by focusing on disciplined underwriting and claims management, utilizing medical provider networks designed to produce superior medical and indemnity outcomes, establishing and maintaining strong, long-term relationships with traditional and specialty insurance agencies, developing important alternative distribution channels, and offering workers' compensation insurance solutions directly to customers.

The company continues to invest in technology to automate business processes and further develop the company’s data analytic capabilities.
Products and Services
Workers' compensation provides insurance coverage for the statutorily prescribed benefits that employers are required to provide to their employees who may be injured or suffer illness in the course of employment. The level of benefits varies by state, the nature and severity of the injury or disease, and the wages of the injured worker. Each state has a statutory, regulatory, and adjudicatory system that sets the amount of wage replacement to be paid, determines the level of medical care required to be provided, establishes the degree of permanent impairment, and specifies the options in selecting healthcare providers. These state laws generally require two types of benefits for injured employees: (a) medical benefits, including expenses related to the diagnosis and treatment of an injury, disease, or both, as well as any required rehabilitation, and (b) indemnity payments, which consist of temporary wage replacement, permanent disability payments, and death benefits to surviving family members.
Disciplined Underwriting
The company’s strategy is to focus on disciplined underwriting and continually pursue profitable growth opportunities across market cycles when presented. The company carefully monitors market trends to assess business opportunities that the company expects will meet its pricing and risk standards. The company’s disciplined underwriting approach, workers' compensation specialization, expertise in underwriting small businesses, and data-driven strategies are critical elements of the company’s culture.
The company executes its underwriting processes through automated systems and experienced underwriters with specific knowledge of the local markets in which the company operates. The company has developed automated underwriting templates for specific classes of business that produce faster quotes when certain underwriting criteria are met. The company’s underwriting guidelines consider many factors, such as type of business, nature of operations, and risk exposures, and are designed to minimize or prevent underwriting of certain classes of business that the company views as being unattractive.
Loss Control Services
The company’s Risk Advisory and Loss Control group manages the company’s programs geared toward helping the company’s small business partners increase workplace safety and provide timely and appropriate care to their injured employees. The company provides expert advice on the root cause of incidents and assistance in the development of policies and programs to help protect workers and navigate the often confusing worker’s compensation process.
Premium Audit
The company conducts premium audits on substantially all of its policyholders annually upon the policy expiration or termination. Premium audits allow the company to comply with applicable state and reporting bureau requirements and to verify that policyholders have accurately reported their payroll and employee job classifications. The company also selectively performs audit reviews and/or update renewal payroll on policies in certain classes of business or if unusual claims are filed or concerns are raised regarding projected annual payrolls, which could result in substantial variances at final audit.
Claims and Medical Case Management
The role of the company’s claims department is to actively and efficiently investigate, evaluate, and pay claims, and to aid injured workers in returning to work in accordance with applicable laws and regulations. The company has implemented rigorous claims guidelines and control procedures in the company’s claims units and has claims operations throughout the markets the company serves. The company also provides medical case management services for those claims that the company determine will benefit from such involvement.
The company utilizes an outcome-based medical network that incorporates predictive analytics to identify medical providers who achieve superior clinical outcomes for the company’s injured workers that allows the company to optimize its provider network and enhance the quality of care. The company has also implemented a proactive pharmacy benefit management program that, along with the company’s outcome-based medical network, focuses on reducing claims costs and accelerating injured workers' return to work. The company has an Injured Employee Hotline that allows employees who are injured at work to receive professional nurse consultation by phone when reporting the claim. This service has proven to reduce overall claims costs and is intended to ensure the injured worker receives appropriate and timely medical care.
In addition to the company’s medical networks, the company works with local vendors, including attorneys, medical professionals, pharmacy benefits managers, and investigators, to bring local expertise to the company’s reported claims. The company has established discounting arrangements with the aforementioned service providers. The company uses preferred provider organizations, bill review services, and utilization management to closely monitor medical costs. The company actively investigates and pursues all types of fraud. The company has implemented a medical provider fraud tool that allows the company to identify suspicious medical billing and activity within the company’s claims. The company also aggressively pursues all subrogation recoveries to mitigate claims costs. Subrogation rights are based upon state and federal laws, as well as the insurance policies the company issues. The company’s fraud and subrogation efforts are handled through dedicated units.
The company utilizes a claim triage predictive model nationally that provides the company with early identification of those claims likely to develop into large losses. Leveraging this information, the company ensures the right resources and strategies are brought to bear on those claims early in the process.
The company’s claims department also provides claims management services for those claims incurred by the Fund, which were assumed by EICN and are subject to the LPT Agreement with dates of injury prior to July 1, 1995. The company receives a management fee from the third party reinsurers equal to 7% of the loss payments on these claims.
Reportable Segment
The company operates its business as a single segment, Insurance Operations, through the company’s wholly owned subsidiaries. In the fourth quarter of 2023, the company developed and executed an integration plan to consolidate the company’s previously segregated direct-to-consumer operations (Cerity) into the company’s mainstream operations, while retaining its digital distribution capabilities. The integration plan, which will allow the company to operate more efficiently and generate cost savings, resulted in a change in the composition of the company’s reportable segments by eliminating any distinction among the company’s former segments, which were: Employers and Cerity.
Workers' Compensation Premiums
The company generally targets select small businesses engaged in low-to-medium hazard industries. The company’s underwriters use their local market expertise and disciplined underwriting to select specific types of businesses and risks within the classes of business the company underwrites that allow the company to generate loss ratios that are better than the industry average.
The company provides workers' compensation insurance throughout the United States, with the exception of four states that are served exclusively by their state funds. The company’s business is concentrated in California.
The company’s premiums are generally a function of the applicable premium rate, the amount of the insured's payroll, and if applicable, a factor reflecting the insured's historical loss experience (experience modification factor).
The company’s premium rates are based upon actuarial analyses for each state in which the company does business, except in administered pricing states, where premium rates are set by state insurance regulators and are adjusted periodically.
Marketing and Distribution
The company markets and sells its workers' compensation insurance products through local, regional, specialty and national insurance agents and brokers; national, regional, and local trade groups and associations; and direct-to-customer interactions.
Traditional Insurance Agents and Brokers
The company establishes and maintains strong, long-term relationships with its vetted and appointed traditional insurance agencies that actively market the company’s products and services. The company offers ease of doing business, provide responsive service, and pay competitive commissions. The company’s sales representatives and underwriters work closely with these agencies to market and underwrite the company’s business. This results in enhanced understanding of the businesses, the risks the company underwrites, and the needs of prospective customers. The company does not delegate underwriting authority to agents or brokers.
The company had approximately 2,500 traditional insurance agencies that marketed and sold the company’s insurance products at December 31, 2023. These agencies generated 67.1% of the company’s in-force premiums at December 31, 2023, and the company’s largest traditional insurance agency generated less than five percent of the company’s in-force premiums at December 31, 2023.
Specialty Agents and Distribution Partners
The company has developed and continue to add other important and emerging distribution channels for the company’s products and services that serve as an alternative to the company’s strong traditional insurance agency channel. These additional channels include distribution partners that utilize partnerships and alliances with entities, such as payroll companies, and health care and property and casualty insurers, as well as digital agents and marketplaces. The company’s workers’ compensation insurance products are jointly offered and marketed with and through the company’s partners and alliances.
Select insurance agencies who possess deep expertise in specialized industries market and sell the company’s insurance products that generally fall outside of the company’s traditional appetite, such as senior care and parcel delivery.
Specialty agents and distribution partners generated 32.9% of the company’s in-force premiums as of December 31, 2023. The company’s strong presence and relationships with these digital and payroll specialty entities allow the company to approach new customers that the company would not otherwise have access to through the company’s traditional insurance agency distribution channel. The bundling of products and services through these relationships contributes to higher retention rates than business generated by the company’s traditional agents, and the company continues to actively seek new partnerships and alliances in these areas.
A significant concentration of the company’s business is generated by the company’s specialty agent ADP. ADP is the largest payroll services provider in the United States. As part of its services, ADP sells the company’s workers' compensation insurance product along with its payroll and accounting services through its insurance agency and field sales staff. ADP generated 16.2% of the company’s in-force premiums as of December 31, 2023. The majority of this business is written through ADP's small business unit, which specializes in accounts from 1 to 50 employees. The company’s relationship with ADP is non-exclusive; however, the company is a key partner for ADP in its selected markets and classes of business.
The company’s digital distribution channel utilizes proprietary application programming interfaces (APIs) to submit, quote and bind applications for workers' compensation insurance. The company’s digital channel is consisted of digital marketplace platforms, as well as appointed digital retail and wholesale agency models. Digital agents generated 5.0% of the company’s in-force premiums as of December 31, 2023. The company continues to actively seek new digital distribution partnerships and expect the company’s existing partnerships to continue to grow in this channel.
Direct-to-Customer
To address the changing buying behaviors of small and micro-businesses, the company continues its commitment to its Cerity brand, which offers digital insurance solutions, including direct-to-customer workers' compensation coverage. Cerity specializes in smaller risks in those classes of business where customers prefer an online experience and offers a digital and mobile-friendly experience that allows small businesses to easily acquire and maintain their policies.
History
Employers Holdings, Inc. was founded in 2000. The company was incorporated in Nevada in 2005.

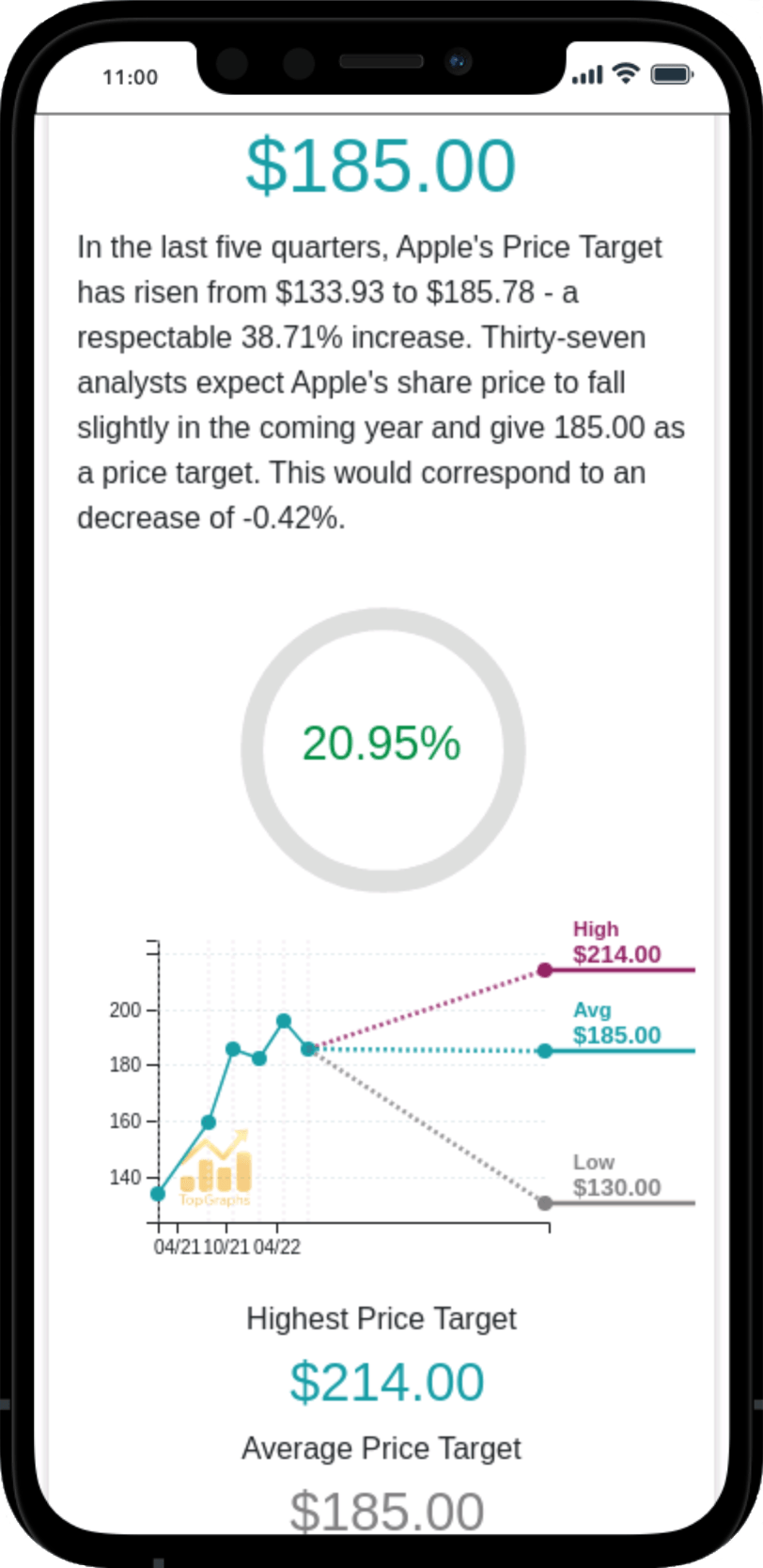
 Stock Value
Stock Value