About American Well
American Well Corporation is a leading enterprise software company digitally enabling hybrid care. The company empowers health providers, payers, and innovators to achieve their digital ambitions, enabling a coordinated experience across in-person, virtual and automated care. The company provides its clients with the core technology and services necessary to successfully develop and distribute digital care programs that meet their strategic, operational, financial and clinical objectives under their own brands.
Amwell pioneered virtual healthcare. Amwell extends digital care beyond telehealth, enabling care across in-person, virtual and automated modalities and providing an open, scalable platform that can flex and grow alongside the company’s clients. The company brings technology and services that facilitate new models of care, strategic partnerships, consistent execution and better outcomes. Together with its clients and innovation partners, the company forges a new hybrid model of care delivery that adapts as needs evolve and makes care more accessible for all.
As of December 31, 2023, the company powered the digital care programs of more than 50 health plans, which collectively represent more than 100 million covered lives, as well as approximately 115 of the nation’s largest health systems.
The company’s enterprise platform and software as a service solutions enable hybrid care delivery by offering its clients products to help weave digital care across all care settings. For health systems, the company’s enterprise platform enables provider-to-provider virtual care for use cases ranging from stroke and acute psychiatry evaluations to virtual nursing and e-sitting. The company’s suite of Carepoint devices can enhance in-person care, whether the clients want to turn existing equipment such as televisions or iPads into digital access points or use Amwell Carepoint carts and peripherals. The company’s enterprise platform also helps extend care outside the care setting by enabling both on-demand and scheduled provider-to-patient care for a range of use cases. This includes, but is not limited to, urgent care, primary care, behavioral health, chronic disease management, and specialty follow-up care. To augment in-person and virtual care, the company’s automated care programs and digital mental health services help clinicians and health plans engage patients, members, and consumers before, after, or in-between visits to improve care plan adherence and prevent costly escalations.
For health plans, employers and government entities, the company’s enterprise platform enables a member-centric hybrid care experience, seamlessly connecting with current technology investments and offering an open architecture that allows simple integration of future innovation. The platform enables a broad set of use cases, including primary, urgent, mental health, specialty, and chronic care. The company’s virtual primary care solution offers a primary care navigation hub that supports a longitudinal care experience for members, integrating virtual visits with digital behavioral health tools and condition-specific automated care programs, with escalation back to virtual and/or in person care, if needed. The company’s urgent care solution helps members conveniently and effectively address unplanned care needs without visiting the emergency department or local urgent care facility.
As of December 31, 2023, approximately 99,500 of the company’s clients’ providers use its enterprise platform and software to serve their patients and members. When needed, it augments and extends its clients’ clinical capabilities with Amwell Medical Group (AMG), a nationwide network of clinical entities with multi-disciplinary providers covering 50 states with 24/7/365 coverage. The AMG network includes a clinical entity with care capabilities that have been accredited by the National Committee for Quality Assurance (NCQA) and a separate clinical entity with psychiatric care capabilities accredited by the Joint Commission.
The Converge platform (Converge) is the latest version of the company’s enterprise platform software. The company designed the platform to be future-ready, reliable, flexible, scalable, secure and fully integrated with other healthcare software systems. Converge offers state-of-the-art data architecture and video capabilities, flexibility and scalability, as well as a user experience focused on the needs of patients, members and providers.
Solution
One Platform, Powering the Care Continuum
Converge, the company’s cloud-based enablement platform, is its go-forward strategy to digitally enable a single, unified, scalable healthcare experience across all care settings. The development of Converge represented a re-platforming by the company to provide its customer base with an improved and more robust solution During the fourth quarter of 2023, 52% of the company’s visits were provided on Converge, which was an increase from 28% in the fourth quarter of 2022.
Converge is designed to remotely implement hybrid care solutions for the company’s clients and grow with them as they broaden their offerings. The platform allows clients the flexibility to build their optimal hybrid care model across a wide variety of use cases based on their unique needs.
With its enterprise platform and software as a service, clients can seamlessly activate additional solutions on Converge as new needs arise, all working together to create a more connected experience for patients and providers.
Health plans typically begin with urgent care, virtual primary care, or behavioral health. Clients also can offer members access to the company’s suite of specialty care programs, including dermatology, musculoskeletal care, second opinion, dermatology, and cardiometabolic care. Converge’s open architecture allows it to integrate with health plans’ and employers’ existing systems and point solutions, connecting the digital care ecosystem and simplifying the member experience.
The company has designed Converge to be future-ready, intuitive and convenient for patients, providers and payers:
Patients and Members—For member or patient-initiated on-demand/urgent care visits, patients can elect to see the next available clinician. For scheduled visits, patients are guided through customizable pre-visit readiness assessments and can enroll themselves and their dependents, enter their medical history, and check insurance coverage. Entering a visit is simple; patients just click on a link they receive in a text message or email. No app download is required. Post visit, patients can access their visit record or share it with other providers in their care team.
Providers—Converge is designed to deliver an easy-to-use provider experience via web or mobile device. Providers access familiar workflows for taking notes, prescribing, referencing clinical treatment guidelines and alerts for gaps in care or referral protocols. They can enroll patients in automated care programs to augment care, when appropriate. Importantly, Converge solutions can be launched directly from within a provider’s EHR system, creating a seamless experience and reducing redundant data entry.
Payers —Access to Converge can be embedded directly into health plan portals, websites, and mobile applications, all using the health plan’s trusted brand. The platform integrates directly with claims and eligibility systems to enable eligibility verification and collection of correct co-insurance payments from patients at the time of the visit. In addition, the platform enables payers to connect their own digital assets, influence member workflows, and present key clinical quality information, such as gaps in care, to providers at the time of a visit. Converge also enables payers with provider networks or integrated delivery networks to seamlessly incorporate their own providers to care delivery programs.
Carepoint Devices and Connections Enable a Variety of Clinical Settings
Amwell Carepoint devices enable healthcare providers to leverage proprietary carts and transform existing tablets and TVs into digital access points in clinical settings, helping to address personnel shortages and access limitations. The company’s proprietary Carepoint devices coupled with its Carepoint Calling technology enables providers to deliver digital care into clinical care locations, such as the emergency department, community hospitals, clinics, and hospital-at-home, as well as into community settings such as retail stores, employer sites, skilled nursing facilities, correctional facilities, and schools. The company’s Virtual Nursing and patient monitoring (eSitter) offerings leverage these Carepoint devices to augment on-site nurse teams with virtual staff, and leverage technology to increase patient safety and nurse efficiencies. These devices are built to rigorous safety and clinical standards and have advanced features including far-end camera controls, fleet monitoring and connectivity to a variety of peripherals, including diagnostic scopes and heart, lungs, stomach and ear examination tools. The company’s Carepoint portfolio supports a range of uses, including multi-way video, phone connectivity and secure messaging to bring care teams to patients and members in the most efficient way possible.
Value-Added Services
The company offers a full suite of paid, supporting services to its clients to enable their hybrid care strategy. AMG contracts with providers across primary and urgent care, behavioral health therapy, acute psychiatry, lactation counseling, and nutrition to provide licensed, reimbursable medical staffing for digital care delivery to its clients. AMG can be used to augment provider capacity during nights, weekends or times of high demand. This nationwide network of clinicians can also fill gaps in specialist coverage in acute hospital settings and enable expanded geographic coverage in cases where state-level licensing requirements restrict the ability of the company’s clients’ own physicians to treat patients outside of their own geographic locations. Additionally, the company provides professional services to facilitate implementation, workflow design, systems integration, and service expansion for all of its products. To help its clients promote adoption and utilization of its products, the company offers patient and provider engagement services.
Competition
The company’s competitors include:
Platform telehealth players, such as Teladoc and Caregility;
Consumer-focused telehealth competitors, such as Included Health and MDLive;
Technology players leveraging horizontal platforms into the healthcare vertical, such as Microsoft, Amazon, and Zoom;
Virtual nursing offerings, such as Care.AI and Avasure;
EHR providers, including Epic, Oracle Health, Allscripts and athenahealth;
Digital patient engagement companies like Twistle, GetWell Loop, and Memora Health;
Digital behavioral health companies, like Ableto, Headspace, Array, and Neuroflow.
Growth Strategies
The key elements of the company’s strategy are to expanding the populations to which its clients offer services; increasing adoption within existing populations; adding new solutions; enabling the sale of new solutions and services for clients to sell to their consumers and B2B customers; expanding their Carepoint suite; investing in platform to continue to expand capabilities; expanding into international markets; and pursuing strategic and complementary assets to support its clients’ needs.
Products
The primary product the company sells is access to its enterprise platform and software via recurring subscriptions. The company sells additional related services and solutions via configurable modules and programs and Carepoint devices and services, including implementation, engagement, cart fleet management and integration. These additional services can be added to any base platform subscription. The company enables the success of the software it sells by also selling access to clinical services on a fee-for-service basis on its platform and through its direct-to-consumer app.
Technology and Operations
The company’s platform, software and services are designed to provide superior patient and provider experiences. The company’s backend architecture also supports security, data exchange, integration with EHRs, other data repositories and third-party devices. Finally, the company offers a portfolio of services to its clients to support their digital care platform. Converge includes clinical services capabilities designed to attract and retain patients, drive operational efficiency, encourage physician engagement, enable digital care delivery for health systems and engage members and lower the cost of care for health plans.
Clinical Services Capabilities
Multiple Digital Practices
Patient care is organized into online practices, analogous to a multi-specialty hospital building, allowing patients to choose from a variety of clinical offerings, ranging from primary to specialty care and from wellness to disease. Practices can be organized by clinical specialty (e.g., primary care, therapy, psychiatry, nutrition), by disease state (e.g., diabetes, asthma, hypertension) or by program type (e.g., smoking cessation, weight loss, wellness). Each practice typically represents a distinct clinical use case with its own associated client branding, patient workflows, associated providers, eligibility and pricing. These practices enable clients to attract patients and members and drive revenue with services they offer.
Visits
For urgent care and walk-in clinic type use cases, patients can seek care on-demand whenever coverage is available (50 states and D.C., 24/7 for urgent care via AMG providers). Patients are routed to the next available provider and can review the provider's credentials and biographical information before deciding whether to connect.
For non-urgent cases, including primary care and specialty care, patients can schedule an appointment time. Appointments can be self-scheduled by patients or scheduled on their behalf by an administrator or provider. Provider availability can be synchronized with a client’s master EHR schedule using the company’s scheduling API, eliminating the need for duplicate, and potentially conflicting scheduling, systems for physical and online appointments.
Alternatively, quick-link scheduled visits functionality allows providers to initiate both scheduled and on-demand visits by sending an email or text message invitation. Visit requests can also be triggered automatically by client-configured analytics and alarms using the company’s Telehealth Now web service. Within a few clicks, patients go from email to live video visit, without ever having to manually register or download any software. This provider-initiated visit functionality is useful for both follow-up and more general population health and care management programs.
Physician Brokerage and Utilization Efficiency
The company’s patented, real-time brokerage engine matches each patient with the list of available and eligible providers, based on licensing requirements and client-configurable clinical, business and regulatory rules.
User Experience
The Converge platform is designed to be a consistent experience across any application, workflow or access point for both providers and patients. The entire use experience is brandable by the client, letting providers and patients know they are meeting under the trusted brand of the healthcare organization they trust, driving brand affinity. Additionally, the modular architecture allows for swappable exchange of the entire A/V experience, allowing different vendors or capabilities such as payments or identity management to be quickly integrated in response to client need.
The user experience also has been designed to allow a patient to easily join a visit through Click to Join features: patients can join video visits by clicking on an email or text message, no registration or download required. Tech checks ensure adequate connectivity, browser compatibility and the correct A/V setting, minimizing the risk of dropped or interrupted visits.
Security and Reliability
Converge has been designed to be secure and scalable; testing is automated and includes security scans, all vetted by the company’s QA team. These scans are also vetted by the company’s dedicated cybersecurity team, which includes security experts who monitor and address issues around the clock. The company also has a full, evidence-grade digital forensics system that provides real-time analysis using multiple cloud forensic tools to its cybersecurity team.
Scalability and Innovation
Converge allows providers to easily expand their use of digital care, taking advantage of highly scalable managed services from best-in-class technology partners. A serverless multi-cloud microservices architecture lets Amwell adapt to any scale of processing power needed to address visit volumes. Clients can quickly implement a unique experience for patients and providers and embed any workflow in their own branded web and mobile solutions with low code / no code custom development. As digital care delivery continues to evolve, Amwell clients and partners have the flexibility and agility to scale virtual care 10x, or 1,000x, as needed.
Interoperability
All data within the platform works with healthcare organizations’ systems and any EHR. Being FHIR-native allows the platform to be interoperable with the entire healthcare ecosystem and creates an open platform for third-party developers.
App Framework
The company has opened Converge to others to build on and expand its abilities. The platform can host and operate applications created by outside developers, whether to serve their own organizations or offer innovations to the company’s large ecosystem. The FHIR APIs at the core of the platform can invoke and give context to any external service, which can then be hosted inside the digital care experience, right in the field of view between the patient and the clinician. This app framework allows clients to deliver better, more efficient access to effective care, helping to close gaps in care, enhance treatment and better enable provider-to-patient relationships.
Technology Back-end Architecture
Secure, Scalable, Hosted Environment
The company uses secures, redundant data centers designed with high levels of availability, redundant subsystems, and compartmentalized security zones. With its platform as a Service digital care solution, there is no need for clients to purchase hardware, install and upgrade software, or manage system operations. The hosted approach also ensures that visit capacity scales without requiring client-side interventions or upgrades. The company manages hosting operations and security from its NOC, which is monitored 24 hours a day. From an operations perspective, the company historically delivers high levels of system uptime across its platform, maintained through its 24/7 Cyber Command Center that monitors its platform around the clock.
Due to the sensitive nature of its client and patient data, the company has invested heavily in data security and protection. The company utilizes a multi-tiered security architecture. All data is secured both in motion and at rest using the latest encryption technologies. The company’s C3 command center constantly monitors for vulnerabilities and intrusions, including using third-party vulnerability and penetration testing. All clinical data usage is HIPAA compliant. The company maintains HITRUST, ISO 27001 and PCI compliance certifications. The company’s system security is regularly evaluated and approved by some of the largest health plans, health systems, financial institutions and technology companies in the world. Amwell has deployed its SilverCloud product on the Defense Health Agency’s production environment as part of its continued work in the Federal sector.
Reporting and Analytics
The company provides a range of standard administrative, utilization and clinical reports. More advanced analytics are user-accessible via the company’s Looker data exploration and discovery business intelligence tool.
Branding and Embeddable Experiences
The company supports client branding and unique client experiences by offering the ability to fully brand its software, as well as to use its APIs and embeddable widgets for both the patient and provider experiences, covering the relevant web and mobile interfaces (iOS and Android). The APIs and embeddable widgets, in turn, allow clients to seamlessly embed its end-to-end patient and provider digital care functionality in their own websites, software and mobile applications. Such embedding is designed to give patients and providers a consistent user experience without having to switch tabs or windows, additional logins or additional app downloads.
For example, some health systems have embedded the company’s solutions in their own patient portals. From a provider perspective, clients are embedding the provider virtual care workflow in their EHRs so that online visits are as easy to schedule and conduct as physical visits.
Sales and Marketing
The company sells its digital care solution through its direct sales organization. The company’s direct sales team consists of enterprise-focused field sales professionals who are organized principally by geography and specialty overlays. The company’s sales operations staff, who support its direct sales team, includes product technology experts, lead generation professionals and sales data experts. The company maintains relationships with key industry participants including media publications, industry analyst firms, benefit consultants, brokers, group purchasing organizations and health plan and health system partners.
Channel partners also play a key role in marketing and selling the company’s products to its client base, primarily focusing on Converge and Carepoint devices. For example, through EHR channel partners the company is able to natively embed its technology into existing health system technology infrastructure which, as a competitive differentiator, may lead to a higher win rate. Carepoint channel partners primarily consist of value-added resellers that have established relationships with health systems and health plans. The company typically generates lower revenues in connection with sales obtained through these channel partner agreements.
Clinical Quality
AMG seeks to provide the highest level of clinical quality and consistency of care. All medical professionals go through a rigorous onboarding and credential checking process. When practicing online, doctors are required to deliver care in a medically appropriate setting. The company offers similar best practices and training to its clients who utilize their own providers. Patients consistently rate AMG providers highly, with an average rating of 4.9 out of 5.0.
AMG's clinical operations team works to standardize virtual medical treatment by creating and maintaining standard operating procedures. This team also monitors waiting room queues and can reassign providers and patients as needed. The team uses analytics to test for appropriateness and efficiency of care as well as prescribing behaviors. AMG's team of nurses uses algorithms to identify potential quality issues and conducts manual reviews of clinical cases, utilizing a random audit process in addition to targeted audits, to ensure high quality care is consistently delivered. Finally, a monthly scorecard is distributed to all AMG providers showing their individual and comparative performance.
Government Regulations
The company is subject to the federal self-referral prohibitions, commonly known as the Stark Law. The company is also subject to the federal Anti-Kickback Statute. The company’s international operations are and will be subject to different, and sometimes more stringent, legal and regulatory requirements, which vary widely by jurisdiction, including anti-corruption laws; economic sanctions laws; various privacy, insurance, tax, tariff and trade laws and regulations; corporate governance, privacy, data protection (including the EU General Data Protection Regulation (GDPR) and the UK General Data Protection Regulation (UK GDPR)), data mining, data transfer, labor and employment, intellectual property, consumer protection and investment laws and regulations; discriminatory licensing procedures; required localization of records and funds; and limitations on dividends and repatriation of capital. In addition, the expansion of the company’s operations into foreign countries increases its exposure to the anti-bribery, anti-corruption and anti-money laundering provisions of U.S. law, including the FCPA, and corresponding foreign laws, including the UK Bribery Act.
The company is subject to regulation by OFAC. As a result of its presence in Europe and some of its customers being located in the European Union and the United Kingdom, the company is subject to applicable international laws and regulations related to privacy and the protection of personal data (including data concerning health), in particular the GDPR and the UK GDPR. The company’s European clinical operations team and its health care clients in Europe are regulated as data controllers under GDPR. Outside Europe, the company is subject to privacy and data protection laws in other locations where it operates including Australia, Canada, and South Africa. These jurisdictions have sectoral health information privacy laws and comprehensive privacy laws similar to GDPR in scope.
Intellectual Property
The company’s patent portfolio consists of approximately 43 patents and 4 pending patent applications related to its software and technology. The company owns and uses trademarks and service marks on or in connection with its services, including both unregistered common law marks and issued trademark registrations in the United States and other geographies.
Seasonality
Visit volumes typically follow the annual flu season, rising during quarter four and quarter one and falling in the summer months. While the company sells to and implement its solutions to clients year-round, it experiences some seasonality in terms of when it enters into agreements with its clients and when it launches solutions to members. The company typically enters into a higher percentage of agreements with new clients, as well as renewal agreements with existing clients, in the first and fourth quarters (year ended December 31, 2023).
History
American Well Corporation was founded in 2006. The company was incorporated under the laws of the state of Delaware in 2006.
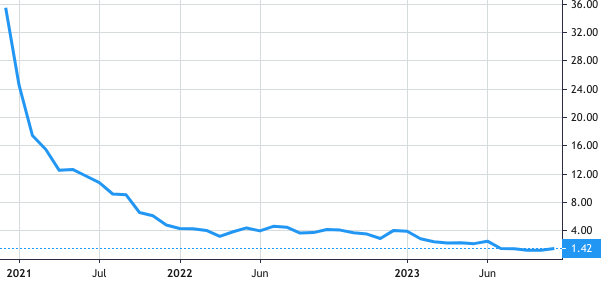
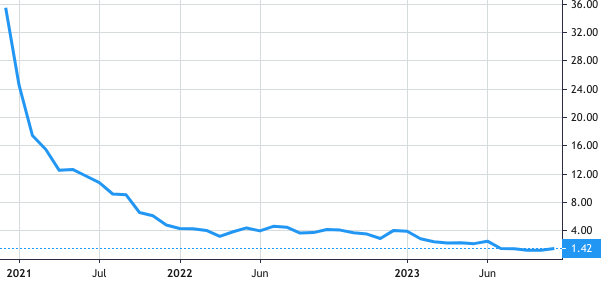
 Stock Value
Stock Value