About CVS Health
CVS Health Corporation, together with its subsidiaries (collectively, CVS Health), is a leading diversified health solutions company reshaping health care to help make healthier happen for more Americans.

The company has more than 1,100 walk-in medical clinics, a leading pharmacy benefits manager with over 110 million plan members with expanding specialty pharmacy solutions and a dedicated senior pharmacy care business serving more than one million patients per year. The company also serves an estimated 35 million people through traditional, voluntary and consumer-directed health insurance products and related services, including expanding Medicare Advantage offerings and a leading standalone Medicare Part D prescription drug plan (PDP).
Segments
The company operates through Health Care Benefits, Pharmacy Services, and Retail/LTC segments.
Health Care Benefits segment
The Health Care Benefits segment operates as one of the nation’s leading diversified health care benefits providers, serving an estimated 35 million people as of December 31, 2022. The Health Care Benefits segment has the information and resources to help members, in consultation with their health care professionals, make more informed decisions about their health care. The Health Care Benefits segment offers a broad range of traditional, voluntary and consumer-directed health insurance products and related services, including medical, pharmacy, dental and behavioral health plans, medical management capabilities, Medicare Advantage and Medicare Supplement plans, PDPs, Medicaid health care management services, and health information technology (HIT) products and services. The Health Care Benefits segment also provided workers’ compensation administrative services through its Coventry Health Care Workers’ Compensation business (Workers’ Compensation business) prior to the sale of this business on July 31, 2020. The Health Care Benefits segment’s customers include employer groups, individuals, college students, part-time and hourly workers, health plans, health care providers (providers), governmental units, government-sponsored plans, labor groups and expatriates.

Health Care Benefits Products and Services
The company refers to insurance products (where it assumes all or a majority of the risk for medical and dental care costs) as Insured and administrative services contract products (where the plan sponsor assumes all or a majority of the risk of medical and dental care costs) as ASC. Health Care Benefits products and services consist of the following:
Commercial Medical: The Health Care Benefits segment offers point-of-service (POS), preferred provider organization (PPO), health maintenance organization (HMO) and indemnity benefit (Indemnity) plans. Commercial medical products also include health savings accounts (HSAs) and consumer-directed health plans that combine traditional POS or PPO and/or dental coverage, subject to a deductible, with an accumulating benefit account (which may be funded by the plan sponsor and/or the member in the case of HSAs). With the launch of Aetna Virtual Primary Care in 2021, eligible members have access to health services remotely, paired with access to in-person visits with providers in the company’s network, including at MinuteClinic locations. Principal products and services are targeted specifically to large multi-site national, mid-sized and small employers, individual insureds and expatriates. The company offers medical stop loss insurance coverage for certain employers who elect to self-insure their health benefits. Under medical stop loss insurance products, the company assumes risk for costs associated with large individual claims and/or aggregate loss experience within an employer’s plan above a pre-set annual threshold. The segment also has a portfolio of additional health products and services that complement its medical products such as dental plans, behavioral health and employee assistance products, provider network access and vision products.
Government Medical: In select geographies, the Health Care Benefits segment offers Medicare Advantage plans, Medicare Supplement plans and prescription drug coverage for Medicare beneficiaries; participates in Medicaid and subsidized Children’s Health Insurance Programs (CHIP); and participates in demonstration projects for members who are eligible for both Medicare and Medicaid (Duals). These Government Medical products are further described below:
Medicare Advantage: Through annual contracts with the U.S. Centers for Medicare & Medicaid Services (CMS), the company offers HMO and PPO products for eligible individuals in certain geographic areas through the Medicare Advantage program. Members typically receive enhanced benefits over traditional fee-for-service Medicare coverage (Original Medicare), including reduced cost-sharing for preventive care, vision and other services. The company offered network-based HMO and/or PPO plans in 46 states and Washington, D.C. in 2022. For certain qualifying employer groups, the company offers Medicare PPO products nationally. When combined with the company’s PDP product, these national PPO plans form an integrated national Insured Medicare product for employers that provides medical and pharmacy benefits.
Medicare PDP: The company is a national provider of drug benefits under the Medicare Part D prescription drug program. All Medicare eligible individuals are eligible to participate in this voluntary prescription drug plan. Members typically receive coverage for certain prescription drugs, usually subject to a deductible, co-insurance and/or co-payment. The company offered PDP plans in all 50 states and Washington, D.C. in 2022.
Medicare Supplement: For certain Medicare eligible members, the company offers supplemental coverage for certain health care costs not covered by Original Medicare. The products included in the Medicare Supplement portfolio help to cover some of the gaps in Original Medicare, and include coverage for Medicare deductibles and coinsurance amounts. The company offered a wide selection of Medicare Supplement products in 49 states and Washington, D.C. in 2022.
Medicaid and CHIP: The company offers health care management services to individuals eligible for Medicaid and CHIP under multi-year contracts with government agencies in various states that are subject to annual appropriations. CHIP are state-subsidized insurance programs that provide benefits for families with uninsured children. The company offered these services on an Insured or ASC basis in 16 states in 2022.
Duals: The company provides health coverage to beneficiaries who are dually eligible for both Medicare and Medicaid coverage. These members must meet certain income and resource requirements in order to qualify for this coverage. The company coordinates 100% of the care for these members and may provide them with additional services in order to manage their health care costs.
The company also has a portfolio of transformative products and services aimed at creating a holistic and integrated approach to individual health and wellness. These products and services complement the Commercial Medical and Government Medical products and aim to provide innovative solutions, create integrated experience offerings and enable enhanced care delivery to customers.
Health Care Benefits Provider Networks
The company contracts with physicians, hospitals and other providers for services they provide to the company’s members. The company uses a variety of techniques designed to help encourage appropriate utilization of medical services (utilization) and maintain affordability of quality coverage. In addition to contracts with providers for negotiated rates of reimbursement, these techniques include creating risk sharing arrangements that align economic incentives with providers, the development and implementation of guidelines for the appropriate utilization and the provision of data to providers to enable them to improve health care quality. As of December 31, 2022, the company’s underlying nationwide provider network had approximately 1.6 million participating providers. Other providers in the company’s provider networks also include laboratory, imaging, urgent care and other freestanding health facilities.
Health Care Benefits Quality Assessment
CMS uses a 5-star rating system to monitor Medicare health care and drug plans and ensure that they meet CMS’s quality standards. CMS uses this rating system to provide Medicare beneficiaries with a tool that they can use to compare the overall quality of care and level of customer service of companies that provide Medicare health care and drug plans. The rating system considers a variety of measures adopted by CMS, including quality of preventative services, chronic illness management and overall customer satisfaction. The company seeks Health Plan accreditation for Aetna Inc. (Aetna) HMO plans from the National Committee for Quality Assurance (NCQA), a private, not-for-profit organization that evaluates, accredits and certifies a wide range of health care organizations. Health care plans seeking accreditation must pass a rigorous, comprehensive review and must annually report on their performance.
Aetna Life Insurance Company (ALIC), a wholly-owned subsidiary of the company, has received nationwide NCQA PPO Health Plan accreditation. As of December 31, 2022, all of the company’s Commercial HMO and all of ALIC’s PPO members who were eligible participated in HMOs or PPOs that are accredited by the NCQA.
The company’s provider selection and credentialing/re-credentialing policies and procedures are consistent with NCQA and URAC, a health care accrediting organization that establishes quality standards for the health care industry, as well as state and federal, requirements. In addition, the company is certified under the NCQA Credentials Verification Organization (CVO) certification program for all certification options and has URAC CVO accreditation.
Quality assessment programs for contracted providers who participate in the company’s networks begin with the initial review of health care practitioners. Practitioners’ licenses and education are verified, and their work history is collected by the company or in some cases by the practitioner’s affiliated group or organization. The company generally requires participating hospitals to be certified by CMS or accredited by The Joint Commission, the American Osteopathic Association, or Det Norske Veritas Healthcare.
The company also offers quality and outcome measurement programs, quality improvement programs, and health care data analysis systems to providers and purchasers of health care services.
Health Care Benefits Information Systems
The Health Care Benefits segment operates and supports an end-to-end suite of information technology platforms to support member engagement, enrollment, health benefit administration, care management, service operations, financial reporting and analytics. The multiple platforms are supported by an integration layer to facilitate the transfer of real-time data. There is continued focus and investment in enterprise data platforms, cloud capabilities, digital products to offer innovative solutions and a seamless experience to the company’s members through mobile and web channels. The company is making concerted investments in emerging technology capabilities such as voice, artificial intelligence and robotics to further automate, reduce cost and improve the experience for all of its constituents. The Health Care Benefits segment is utilizing the full breadth of the company’s assets to build enterprise technology that will help guide its members through their health care journey, provide them a high level of service, enable healthier outcomes and encourage them to take next best actions to lead healthier lives.
Health Care Benefits Customers
Medical membership is dispersed throughout the United States, and the company also serves medical members in certain countries outside the United States. The company offers a broad range of traditional, voluntary and consumer-directed health insurance products and related services, many of which are available nationwide. Depending on the product, the company markets to a range of customers, including employer groups, individuals, college students, part-time and hourly workers, health plans, providers, governmental units, government-sponsored plans, labor groups and expatriates.
The company markets both Commercial Insured and ASC products and services primarily to employers that sponsor the company’s products for the benefit of their employees and their employees’ dependents. Typically, employers pay all of the monthly premiums to the company and, through payroll deductions, obtain reimbursement from employees for a percentage of the premiums that is determined by each employer. Some Health Care Benefits products are sold directly to employees of employer groups on a fully employee-funded basis. In some cases, the company bills the covered individual directly. In addition, effective January 2022, the company entered the individual public health insurance exchanges (Public Exchanges) in eight states through which it sells Insured plans directly to individual consumers. The company entered Public Exchanges in four additional states effective January 2023.
The company offers Insured Medicare coverage on an individual basis, as well as through employer groups to their retirees. Medicaid and CHIP members are enrolled on an individual basis. The company also offers Insured health care coverage to members who are dually-eligible for both Medicare and Medicaid.
Health Care Benefits products are sold through the company’s sales personnel; independent brokers, agents and consultants who assist in the production and servicing of business; as well as private health insurance exchanges (Private Exchanges) and Public Exchanges (together with Private Exchanges, Insurance Exchanges). For large employers or other entities that sponsor the company’s products (plan sponsors), independent consultants and brokers are frequently involved in employer health plan selection decisions and sales. In some instances, the company may pay commissions, fees and other amounts to brokers, agents, consultants and sales representatives who place business with the company. In certain cases, the customer pays the broker for services rendered, and the company may facilitate that arrangement by collecting the funds from the customer and transmitting them to the broker. The company supports marketing and sales efforts with an advertising program that may include television, radio, billboards, print media and social media, supplemented by market research and direct marketing efforts.
The U.S. federal government is a significant customer of the Health Care Benefits segment through contracts with CMS for coverage of Medicare-eligible individuals and federal employee-related benefit programs. Other than the contracts with CMS, the Health Care Benefits segment is not dependent upon a single customer or a few customers the loss of which would have a significant effect on the earnings of the segment. The loss of business from any one or a few independent brokers or agents would not have a material adverse effect on the earnings of the Health Care Benefits segment.
Health Care Benefits Pricing
The company has Medicare Advantage and PDP contracts with CMS to provide HMO, PPO and prescription drug coverage to Medicare beneficiaries in certain geographic areas. Under these annual contracts, CMS pays the company a fixed per member (or capitation) payment and/or a portion of the premium, both of which are based on membership and adjusted for demographic and health risk factors. CMS also considers inflation, changes in utilization patterns and average per capita fee-for-service Medicare costs in the calculation of the fixed capitation payment or premium. PDP contracts also provide a risk-sharing arrangement with CMS to limit the company’s exposure to unfavorable expenses or benefit from favorable expenses. Amounts payable to the company under the Medicare arrangements are subject to annual revision by CMS, and the company elects to participate in each Medicare service area or region on an annual basis. Premiums paid to the company for Medicare products are subject to federal government reviews and audits, which can result, and has resulted, in retroactive and prospective premium adjustments and refunds to the government and/or members. In addition to payments received from CMS, some Medicare Advantage products and all PDP products require a supplemental premium to be paid by the member or sponsoring employer. In some cases, these supplemental premiums are adjusted based on the member’s income and asset levels.
The company offers HMO and consumer-directed medical and dental plans to federal employees under the Federal Employees Health Benefits (FEHB) Program and the Federal Employees Dental and Vision Insurance Program. Premium rates and fees for those plans are subject to federal government review and audit, which can result, and have resulted, in retroactive and prospective premium and fee adjustments and refunds to the government and/or members.
Health Care Benefits Seasonality
The Health Care Benefits segment’s quarterly operating income progression is impacted by the seasonality of benefit costs which generally increase during the year as Insured members progress through their annual deductibles and out-of-pocket expense limits; and the seasonality of operating expenses, which are generally the highest during the fourth quarter due primarily to spending to support readiness for the start of the upcoming plan year and marketing associated with Medicare annual enrollment.
During the year ended December 31, 2022, the impact of COVID-19 within the Health Care Benefits segment has generally stabilized as a result of the company’s ability to capture COVID-19 related medical costs in pricing, and the segment has experienced a return to a more normal seasonality pattern, as described above.
Health Care Benefits Competition
The largest competitor in Medicare products is Original Medicare. The Health Care Benefits segment’s ASC plans compete primarily with other large commercial health care benefit companies, numerous for-profit and not-for-profit organizations operating under licenses from the Blue Cross and Blue Shield Association and TPAs.
Health Care Benefits Reinsurance
The company has several reinsurance agreements with non-affiliated insurers that relate to Health Care Benefits insurance policies. The company entered into these contracts to reduce the risk of catastrophic losses which in turn reduces capital and surplus requirements. The company frequently evaluates reinsurance opportunities and refines its reinsurance and risk management strategies on a regular basis.
Pharmacy Services segment
The Pharmacy Services segment provides a full range of PBM solutions, including plan design offerings and administration, formulary management, retail pharmacy network management services and mail order pharmacy. In addition, through the Pharmacy Services segment, the company provides specialty pharmacy and infusion services, clinical services, disease management services, medical spend management and pharmacy and/or other administrative services for providers and federal 340B drug pricing program covered entities (Covered Entities). The company operates a group purchasing organization that negotiates pricing for the purchase of pharmaceuticals and rebates with pharmaceutical manufacturers on behalf of its participants. The company also provides various administrative, management and reporting services to pharmaceutical manufacturers. The Pharmacy Services segment’s clients are primarily employers, insurance companies, unions, government employee groups, health plans, PDPs, Medicaid managed care (Managed Medicaid) plans, plans offered on Insurance Exchanges and other sponsors of health benefit plans throughout the United States and Covered Entities. The Pharmacy Services segment operates retail specialty pharmacy stores, specialty mail order pharmacies, mail order dispensing pharmacies, compounding pharmacies and branches for infusion and enteral nutrition services. During the year ended December 31, 2022, the company’s PBM filled or managed 2.3 billion prescriptions on a 30-day equivalent basis.
PBM Services
The company dispenses prescription drugs directly through its mail order dispensing and specialty mail order pharmacies and through pharmacies in its retail network. All prescriptions processed by the company are analyzed, processed and documented by the company’s proprietary prescription management systems. These systems provide essential features and functionality to allow plan members to utilize their prescription drug benefits. These systems also streamline the process by which prescriptions are processed by staff and network pharmacists by enhancing review of various items through automation, including plan eligibility, early refills, duplicate dispensing, appropriateness of dosage, drug interactions or allergies, over-utilization and potential fraud.
Plan Design Offerings and Administration
The company assists its PBM clients in designing pharmacy benefit plans that help improve health outcomes while minimizing the costs to the client. The company also assists PBM clients in monitoring the effectiveness of their plans through frequent, informal communications, the use of proprietary software, as well as through formal annual, quarterly and sometimes monthly performance reviews. The company administers pharmacy benefit plans for clients who contract with it to facilitate prescription drug coverage and claims processing for their eligible plan members. The company also provides administrative services for Covered Entities.
The company makes recommendations to help PBM clients design benefit plans that promote the use of lower cost, clinically appropriate drugs and helps its PBM clients control costs by recommending plan designs that encourage the use of generic equivalents of brand name drugs when such equivalents are available. Clients also have the option, through plan design, to further lower their pharmacy benefit plan costs by setting different member payment levels for different products on their drug lists or formularies, which helps guide members to choose lower cost alternatives through appropriate financial incentives.
Formulary Management
The company utilizes an independent panel of doctors, pharmacists and other medical experts, referred to as the CVS Caremark National Pharmacy and Therapeutics Committee, to review and approve the selection of drugs that meet the company’s standards of safety and efficacy for inclusion on one of the company’s template formularies. The company’s formularies provide recommended products in numerous drug classes to help ensure member access to clinically appropriate drugs with alternatives within a class under the client’s pharmacy benefit plan, while helping to drive the lowest net cost for clients that select one of the company’s formularies. To help improve clinical outcomes for members and clients, the company conducts ongoing, independent reviews of all drugs, including those appearing on the formularies and generic equivalent products. Many of the company’s clients choose to adopt a template formulary offering as part of their plan design. PBM clients are given capabilities to offer real time benefits information for a member’s specific plan design, provided digitally at the point of prescribing, at the CVS pharmacy and directly to members.
Retail Pharmacy Network Management Services
The company maintains a national network of retail pharmacies, consisting of approximately 40,000 chain pharmacies (which include CVS pharmacy locations) and approximately 26,000 independent pharmacies, in the United States, including Puerto Rico, the District of Columbia, Guam and the U.S. Virgin Islands. When a customer fills a prescription in a retail pharmacy, the pharmacy sends prescription data electronically to the company from the point-of-sale. This data interfaces with the company’s proprietary prescription management systems, which verify relevant plan member data and eligibility, while also performing a drug utilization review to help evaluate clinical appropriateness and safety and confirming that the pharmacy will receive payment for the prescription.
Mail Order Pharmacy Services
The Pharmacy Services segment operates mail order dispensing pharmacies in the United States. Plan members or their prescribers submit prescriptions or refill requests, primarily for maintenance medications, to these pharmacies, and staff pharmacists review these prescriptions and refill requests with the assistance of the company’s prescription management systems. This review may involve communications with the prescriber and, with the prescriber’s approval when required, can result in generic substitution, therapeutic interchange or other actions designed to help reduce cost and/or improve quality of treatment. The company’s mail order dispensing pharmacies have been awarded Mail Service Pharmacy accreditation from URAC.
Specialty Pharmacy and Infusion Services
The Pharmacy Services segment operates specialty mail order pharmacies, retail specialty pharmacy stores and branches for infusion and enteral nutrition services in the United States. The specialty mail order pharmacies are used for delivery of advanced medications to individuals with chronic or genetic diseases and disorders. The company’s specialty mail order pharmacies have been awarded Specialty Pharmacy accreditation from URAC. Substantially all of the company’s specialty mail order pharmacies also have been accredited by The Joint Commission and the Accreditation Commission for Health Care (ACHC), which are independent, not-for-profit organizations that accredit and certify health care programs and organizations in the United States. The ACHC accreditation includes an additional accreditation by the Pharmacy Compounding Accreditation Board, which certifies compliance with the highest level of pharmacy compounding standards.
Clinical Services
The company offers multiple clinical programs and services to help clients manage overall pharmacy and health care costs in a clinically appropriate manner. These programs are primarily designed to promote better health outcomes and to help target inappropriate medication utilization and non-adherence to medication, each of which may result in adverse medical events that negatively affect member health and client pharmacy and medical spend. These programs include utilization management (UM), medication management, quality assurance, adherence and counseling programs to complement the client’s plan design and clinical strategies. To help address prescription opioid abuse and misuse, the company introduced an industry-leading UM approach that limits to seven days the supply of opioids dispensed for certain acute prescriptions for patients who are new to therapy, limits the daily dosage of opioids dispensed based on the strength of the opioid and requires the use of immediate-release formulations of opioids before extended-release opioids are dispensed. The company’s Pharmacy Advisor program facilitates pharmacist counseling, both face-to-face and over the telephone, to help participating plan members with certain chronic diseases, such as diabetes and cardiovascular conditions, to identify gaps in care, adhere to their prescribed medications and manage their health conditions. The company also has digital connectivity that helps to lower drug costs for patients by providing expanded visibility to lower cost alternatives through enhanced analytics and data sharing.
Disease Management Programs
The company’s clinical programs and services utilize advanced protocols and offer clients convenience in working with providers and other third parties. The Company’s care management program covers diseases, such as rheumatoid arthritis, Parkinson’s disease, epilepsy and multiple sclerosis and is accredited by the NCQA. The company’s UM program covers similar diseases and is accredited by the NCQA and URAC.
Medical Benefit Management
The company’s NovoLogix online preauthorization tool helps identify and capture cost savings opportunities for specialty drugs billed under the medical benefit by identifying outliers to appropriate dosages and costs, and helps to ensure clinically appropriate use of specialty drugs.
Group Purchasing Organization Services
The company operates a group purchasing organization that negotiates pricing for the purchase of pharmaceuticals and rebates with pharmaceutical manufacturers on behalf of its participants. The company also provides various administrative, management and reporting services to pharmaceutical manufacturers.
Pharmacy Services Information Systems
The Pharmacy Services segment’s claim adjudication platform incorporates architecture that centralizes the data generated from filling mail order prescriptions, adjudicating retail pharmacy claims and delivering other solutions to PBM clients. The Health Engagement Engine technology and proprietary clinical algorithms help connect various parts of the enterprise and serve an essential role in cost management and health improvement, leveraging cloud-native technologies and practices. This capability transforms pharmacy data into actionable interventions at key points of care, including in retail, mail and specialty pharmacies, as well as in customer care call center operations, leveraging the company’s enterprise data platform to improve the quality of care. The technology leverages assisted artificial intelligence to deliver insights to the business and bring automation to otherwise manual tasks. Specialty services also connects with the company’s claim adjudication platform and various health plan adjudication platforms with a centralized architecture servicing many clients and members. Operating services, such as Specialty Expedite, provide an interconnected onboarding solution for specialty medications and branding solutions ranging from fulfillment to total patient management. These services are managed through the company’s new innovative specialty workflow and web platform.
Pharmacy Services Clients
The company’s Pharmacy Services clients are primarily employers, insurance companies, unions, government employee groups, health plans, PDPs, Managed Medicaid plans, plans offered on Insurance Exchanges, other sponsors of health benefit plans throughout the United States and Covered Entities. Pharmaceuticals are provided to eligible members in benefit plans maintained by clients and utilize the company’s information systems, among other things, to help perform safety checks, drug interaction screening and identify opportunities for generic substitution. Substantially all of the Pharmacy Services segment’s revenues are generated from dispensing and managing prescription drugs to eligible members in benefit plans maintained by clients.
Pharmacy Services Seasonality
The majority of Pharmacy Services segment revenues are not seasonal in nature.
Pharmacy Services Competition
The Pharmacy Services segment has a significant number of competitors offering PBM services, including large, national PBM companies (e.g., Prime Therapeutics and MedImpact), PBMs owned by large national health plans (e.g., the Express Scripts business of Cigna Corporation and the OptumRx business of UnitedHealth) and smaller standalone PBMs.
Retail/LTC segment
The Retail/LTC segment sells prescription drugs and a wide assortment of health and wellness products and general merchandise, provides health care services through its MinuteClinic walk-in medical clinics, provides medical diagnostic testing, administers vaccinations for illnesses, such as influenza, COVID-19 and shingles and conducts long-term care pharmacy (LTC) operations, which distribute prescription drugs and provide related pharmacy consulting and other ancillary services to long-term care facilities and other care settings. As of December 31, 2022, the Retail/LTC segment operated more than 9,000 retail locations, more than 1,100 MinuteClinic locations, as well as online retail pharmacy websites, LTC pharmacies and on-site pharmacies. During the year ended December 31, 2022, the Retail/LTC segment filled 1.6 billion prescriptions on a 30-day equivalent basis. For the year ended December 31, 2022, the company dispensed approximately 26.8% of the total retail pharmacy prescriptions in the United States.
Retail/LTC Products and Services
A typical retail store sells prescription drugs and a wide assortment of high-quality, nationally advertised brand name and proprietary brand merchandise. Pharmacy locations may also contract with Covered Entities under the federal 340B drug pricing program. Front store categories include over-the-counter drugs, consumer health products, beauty products and personal care products. The company purchases merchandise from numerous manufacturers and distributors. LTC operations include distribution of prescription drugs and related consulting and ancillary services. The company’s MinuteClinic locations offer a variety of health care services.
Retail/LTC revenues by major product group are as follows:
Pharmacy
Pharmacy revenues represented approximately three-fourths of Retail/LTC segment revenues in 2022.
Front Store
Front store revenues reflect the company’s strategy of innovating with new and unique products and services, using innovative personalized marketing and adjusting the mix of merchandise to match customers’ needs and preferences. A key component of the front store strategy is the ExtraCare card program, which is one of the largest and most successful retail loyalty programs in the United States. The ExtraCare program allows the company to balance marketing efforts so it can reward its best customers by providing them with automatic sale prices, customized coupons, ExtraBucks® rewards and other benefits. The company also offers a subscription-based membership program, CarePass, under which members are entitled to a suite of benefits delivered over the course of the subscription period, as well as a promotional reward that can be redeemed for future goods and services. The company continues to launch and enhance new and exclusive brands to create unmatched offerings in beauty products and deliver other unique product offerings, including a full range of high-quality proprietary brand products that are only available through CVS stores. The company carries approximately 5,500 proprietary brand products, which accounted for approximately 21% of front store revenues during 2022.
MinuteClinic
As of December 31, 2022, the company operated more than 1,100 MinuteClinic locations in the United States. The clinics are staffed by nurse practitioners and physician assistants who utilize nationally established guidelines to deliver a variety of health care services. Payors value these clinics because they provide convenient, high-quality, cost-effective care, in many cases offering an attractive alternative to more expensive sites of care. MinuteClinic also offers virtual care services to connect customers with licensed providers to provide access to health services remotely. MinuteClinic is collaborating with the Health Care Benefits and Pharmacy Services segments to help meet the needs of the company’s health plan and client plan members by offering programs that can improve member health and lower costs. MinuteClinic also maintains relationships with leading hospitals, clinics and physicians in the communities the company serves to support and enhance quality, access and continuity of care.
On-site Pharmacies
The company also operates a limited number of pharmacies located at client sites, which provide certain health plan members and customers with a convenient alternative for filling their prescriptions and receiving vaccinations, including the COVID-19 vaccination.
Medical Diagnostic Testing
The company offers medical diagnostic testing primarily through its testing sites located at CVS pharmacy locations, in its MinuteClinic locations, at community-based testing sites in underserved areas and through its Return Ready solution.
Long-term Care Pharmacy Operations
The Retail/LTC segment provides LTC pharmacy services through the Omnicare business. Omnicare’s customers consist of skilled nursing facilities, assisted living facilities, independent living communities, hospitals, correctional facilities, and other health care service providers. The company provides pharmacy consulting, including monthly patient drug therapy evaluations, to assist in compliance with state and federal regulations and provide proprietary clinical and health management programs. It also provides pharmaceutical case management services for retirees, employees and dependents who have drug benefits under corporate-sponsored health care programs.
Community Location Development
CVS Health’s community health destinations are an integral part of its ability to meet the needs of consumers and maintain its leadership position in the changing health care landscape. When paired with its rapidly expanding digital presence, the company’s physical presence in thousands of communities across the country represents a competitive advantage by allowing it to develop deep and trusted relationships through everyday engagement in consumer health. The company’s community health destinations have played, and will continue to play, a key role in the company’s continued growth and success. During 2022, the company opened approximately 40 new locations, relocated 4 locations and closed approximately 300 locations.
The company’s continuous assessment of its national footprint is an essential component of competing effectively in the current health care environment. On an ongoing basis, the company evaluates changes in population, consumer buying patterns and future health needs to assess the ability of its existing stores and locations to meet the needs of its consumers and the business.
Retail/LTC Information Systems
The company has continued to invest in information systems to enable it to deliver exceptional customer service, enhance safety and quality, and expand patient care services while lowering operating costs. The proprietary WeCARE Workflow tool supports pharmacy teams by prioritizing work to meet customer expectations, facilitating prescriber outreach, and seamlessly integrating clinical programs. This solution delivers improved efficiency and enhances customer experience, as well as provides a framework to accommodate the evolution of pharmacy practice and the expansion of clinical programs. The company’s Health Engagement Engine technology and data science clinical algorithms enable the company to help identify opportunities for pharmacists to deliver face-to-face counseling regarding patient health and safety matters, including medication adherence issues, gaps in care and management of certain chronic health conditions. The company’s digital strategy is to empower the consumer to navigate their pharmacy experience and manage their condition through integrated online and mobile solutions that offer utility and convenience. The company’s LTC digital technology suite, Omniview, improves the efficiency of customers’ operations with tools that include executive dashboards, pre-admission pricing, electronic ordering of prescription refills, proof-of-delivery tracking, access to patient profiles, receipt and management of facility bills, and real-time validation of Medicare Part D coverage, among other capabilities.
Through the collaboration of its digital and technical teams, the company has established critical tools which enable patients to schedule diagnostic testing and vaccination appointments through CVS.com and MinuteClinic.com. Key elements of the offerings include landing pages which highlight services and answer common questions, screening capabilities to determine patient eligibility, service location locator and appointment selection tools to efficiently identify the requested service on a specified date, time, and location and registration pages to collect required patient information, accelerating the administration of the test or vaccine once at the store. Once scheduled, the tools provide the user with instructions and notifications, including SMS text message and email reminders, and, following administration, also provide digital results for tests and records for vaccinations, enabling patients to view and save their medical records for convenient access at a later point.
Retail/LTC Customers
The success of the Retail/LTC segment’s businesses is dependent upon the company’s ability to establish and maintain contractual relationships with pharmacy benefit managers and other payors on acceptable terms. Substantially all of the Retail/LTC segment’s pharmacy revenues are derived from pharmacy benefit managers, managed care organizations (MCOs), government funded health care programs, commercial employers and other third-party payors.
Retail/LTC Seasonality
During the year ended December 31, 2022, the customary quarterly operating income progression in the Retail/LTC segment continued to be impacted by COVID-19. During the first quarter, the company saw high volumes of administration of COVID-19 vaccinations, as well as demand for OTC test kits in the front store, particularly in the beginning of the year when the Omicron variant incidence was high. In addition, the company administered the highest quarterly volume of COVID-19 diagnostic tests of 2022 during the first quarter, however a decline compared to the prior year. During the second and third quarters, the company continued to generate earnings from the sale of OTC test kits, as customers performed more in-home testing versus diagnostic testing, in addition to earnings from the continued administration of COVID-19 diagnostic testing and vaccinations, albeit at lower levels than those experienced in the first quarter. During the fourth quarter, the company saw an increase in COVID-19 vaccine administration from the prior quarter related to the bivalent COVID-19 booster.
Competition
In the areas it serves, the company competes with other drugstore chains (e.g., Walgreens and Rite Aid), supermarkets, discount retailers (e.g., Walmart), independent pharmacies, restrictive pharmacy networks, internet companies (e.g., Amazon), membership clubs, retail health clinics, urgent care and primary care offices, as well as mail order dispensing pharmacies. The company’s largest LTC pharmacy competitor nationally is PharMerica.
Business Strategy
The company seeks to reimagine the consumer healthcare experience to make it easier and more affordable to live a healthier life. This means delivering solutions that are more personalized, simpler to use, and increasingly digital so that consumers can receive care when, where and how they desire. The company is a leader in key segments of health care through its foundational businesses and is seeking to create new sources of value by expanding into next generation care delivery and health services, with a goal of improving satisfaction levels for both providers and consumers.
Government Regulation
The Families First Coronavirus Response Act (the Families First Act) and the Coronavirus Aid, Relief, and Economic Security Act (the CARES Act) were enacted in March 2020. Each of the Families First Act and the CARES Act requires the company to provide coverage for coronavirus disease 2019 (COVID-19) related medical services, in many cases without member cost-sharing, in its Insured Health Care Benefits products.
In addition to the Families First Act, the CARES Act, and the American Rescue Plan Act, the company continues to experience new legislation, regulation, directives, orders and other requirements from federal, state, county and municipal authorities related to the COVID-19 pandemic.
In addition to the Families First Act, the CARES Act, and the American Rescue Plan Act, the company has experienced legislation, regulation, directives, orders and other requirements from federal, state, county and municipal authorities related to the COVID-19 pandemic.
The company is subject to various federal and state laws concerning its submission of claims and other information to Medicare, Medicaid and other federal and state government-sponsored health care programs. Potential sanctions for violating these laws include recoupment or reduction of government reimbursement amounts, civil penalties, treble damages, and exclusion from participation in government health care programs. Such laws include the federal False Claims Act (the False Claims Act), the federal anti-kickback statute (the AKS), state false claims acts and anti-kickback statutes in most states, the federal ‘Stark Law’ and related state laws.
The company’s Medicare Advantage and PDP products are heavily regulated by CMS. The American Recovery and Reinvestment Act of 2009 requires the company and other covered entities to report any breaches of protected health information (PHI) to impacted individuals and to the HHS (the U.S. Department of Health and Human Services) and to notify the media in any states where 500 or more people are impacted by the unauthorized release or use of or access to PHI.
Complying with additional state requirements requires the company to make additional investments beyond those the company has made to comply with the federal Health Insurance Portability and Accountability Act of 1996 and the regulations issued thereunder and the Gramm-Leach-Bliley Act.
The company is subject to a variety of intersecting federal and state statutes and regulations that govern the wholesale distribution of drugs; operation of retail, specialty, infusion, LTC and mail order pharmacies; licensure of facilities and professionals, including pharmacists, technicians, nurses and other health care professionals; registration of facilities with the U.S. Drug Enforcement Administration (the ‘DEA’) and analogous state agencies that regulate controlled substances; packaging, storing, shipping and tracking of pharmaceuticals; repackaging of drug products; labeling, medication guides and other consumer disclosures; interactions with prescribers and health care professionals; compounding of prescription medications; dispensing of controlled and non-controlled substances; counseling of patients; transfers of prescriptions; advertisement of prescription products and pharmacy services; security; inventory control; recordkeeping; reporting to Boards of Pharmacy, the U.S. Food and Drug Administration (the ‘FDA’), the U.S. Consumer Product Safety Commission, the DEA and related state agencies; and other elements of pharmacy practice.
The states of domicile of the company’s regulated subsidiaries have statutory risk-based capital (RBC) requirements for health and other insurance companies and HMOs based on the National Association of Insurance Commissioners’ (the ‘NAIC’) Risk-Based Capital for Insurers Model Act (the ‘RBC Model Act’).
The Employee Retirement Income Security Act of 1974 (ERISA) provides for comprehensive federal regulation of certain employee pension and benefit plans, including private employer and union sponsored health plans and certain other plans that contract with the company to provide PBM services. Some of the company’s health and related benefits and large case pensions products and services and related fees also are subject to potential issues raised by judicial interpretations relating to ERISA.
The company’s subsidiaries contract with the Office of Personnel Management (the OPM) to provide managed health care services under the FEHB program in their service areas. The company also has a contractual arrangement with carriers for the FEHB program, such as the BlueCross BlueShield Association, to provide pharmacy services to federal employees, postal workers, annuitants, and their dependents under the Government-wide Service Benefit Plan, as authorized by the FEHB Act and as part of the FEHB program. Additionally, the company manages certain FEHB plans on a cost-plus basis. These arrangements subject the company to certain aspects of the FEHB Act, and other federal regulations, such as the FEHB Acquisition Regulation, that otherwise would not be applicable to the company. The OPM also is auditing the company and its other contractors to, among other things, verify that plans meet their applicable FEHB program-specific MLR and the premiums established under the OPM’s Insured contracts and costs allocated pursuant to the OPM’s cost-based contracts are in compliance with the requirements of the applicable FEHB program.
The company’s international operations are subject to different, and sometimes more stringent, legal and regulatory requirements, which vary widely by jurisdiction, including anti-corruption laws; economic sanctions laws; various privacy, insurance, tax, tariff and trade laws and regulations; corporate governance, privacy, data protection (including the EU’s General Data Protection Regulation which began to apply across the EU during 2018), data mining, data transfer, labor and employment, intellectual property, consumer protection and investment laws and regulations; discriminatory licensing procedures; compulsory cessions of reinsurance; required localization of records and funds; higher premium and income taxes; limitations on dividends and repatriation of capital; and requirements for local participation in an insurer’s ownership. In addition, the presence of operations in foreign countries potentially increases the company’s exposure to the anti-bribery, anti-corruption and anti-money laundering provisions of U.S. law, including the FCPA, and corresponding foreign laws, including the U.K. Bribery Act 2010 (the UK Bribery Act).
The company also is subject to applicable anti-corruption laws of the jurisdictions in which it operates. In many countries outside the United States, health care professionals are employed by the government. Therefore, the company’s dealings with them are subject to regulation under the FCPA. Violations of the FCPA and other anti-corruption laws may result in severe criminal and civil sanctions, as well as other penalties, and there continues to be a heightened level of FCPA enforcement activity by the U.S. Securities and Exchange Commission (the SEC) and the DOJ.
Certain lines of the company’s businesses are subject to Treasury anti-money laundering regulations. The company also is subject to regulation by the Office of Foreign Assets Control of the U.S. Department of Treasury (OFAC).
The FDA regulates the company’s compounding pharmacy and clinical research operations. In addition, the FDA regulates the company’s activities as a distributor of store brand products.
The ACA expanded the premium rate review process by, among other things, requiring the company’s Commercial Insured rates to be reviewed for reasonableness at either the state or the federal level.
The company’s Medicaid, dual eligible and dual eligible special needs plan products also are heavily regulated by CMS and state Medicaid agencies, which have the right to audit the company’s performance to determine compliance with CMS contracts and regulations.
The company’s PBM activities are also regulated directly and indirectly at the federal and state levels, including being subject to the False Claims Act and state false claims acts and the AKS and state anti-kickback laws.
History
CVS Health Corporation was incorporated in Delaware in 1996.

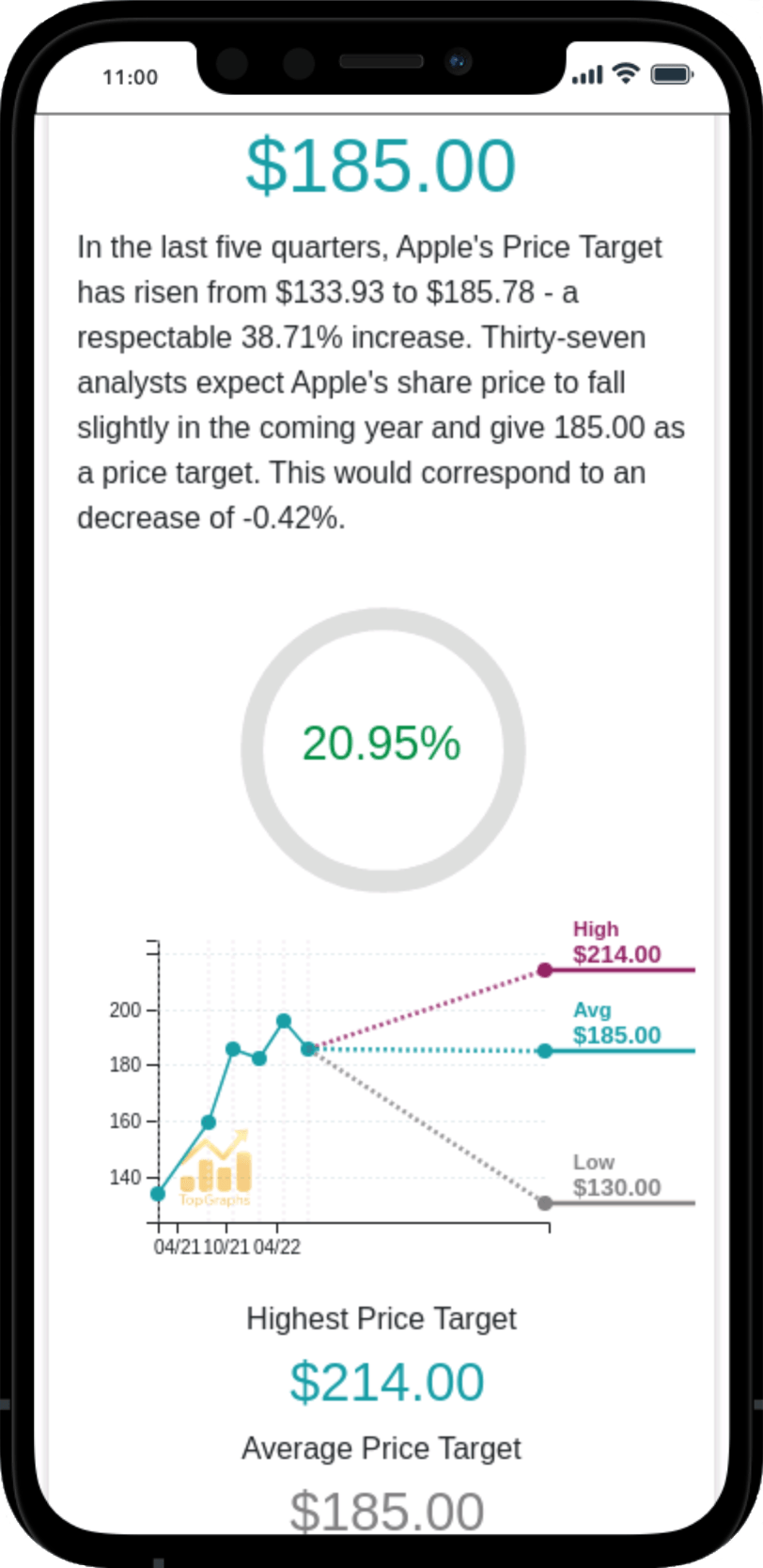
 Stock Value
Stock Value