About The Cigna Group
The Cigna Group (Cigna), together with its subsidiaries, operates as a global health company.

The company has two growth platforms: Evernorth Health Services and Cigna Healthcare. Evernorth Health Services is the company’s pharmacy, care and benefits solution that is highly attractive to the company’s clients and partners because of the depth of its capabilities and expertise. Evernorth Health Services also enables the company to deepen existing relationships across its entire book of business. Cigna Healthcare is the health benefits provider of The Cigna Group, serving customers and clients for the company’s U.S. Commercial, U.S. Government and International Health operating segments; and it allows the company to harness its partnership relationship with physicians to deliver affordable and coordinated health care to employers and individuals.
Together, Evernorth Health Services and Cigna Healthcare provide a strong and diverse foundation that allows the company to capitalize on growth opportunities by leading with the company’s strengths – medical and pharmacy solutions – and then expanding those relationships by addressing additional client needs and innovating and delivering new services and solutions.
The company also has a variety of accelerated growth businesses, both scaled and emerging, which build upon the company’s foundational relationships or provide exposure to adjacent high-growth areas. The company’s cross-enterprise leverage provides the company with an opportunity to unlock even more value as the combined power of the franchise is unleashed.
The company’s portfolio of offerings solves diverse challenges across the health care system. The company offers a differentiated set of pharmacy, medical, behavioral, dental and supplemental products and services, primarily through two growth platforms: Evernorth Health Services and Cigna Healthcare. The company’s capabilities include a broad portfolio of solutions and services, some of which can be offered on a stand-alone basis; integrated behavioral, medical and pharmacy management solutions; leading specialty pharmacy, clinical and care management expertise; and advanced analytics that help the company engage more meaningfully with individuals, the plan sponsors the company serve and its provider partners.
The company improves whole-person health, in body and mind by treating physical and behavioral health together to improve outcomes and by providing early behavioral and lifestyle interventions. The company connects care for the most pressing conditions by closing gaps between hospitals, primary care providers, specialists and other health care providers. The company also develops personalized treatment paths across every dimension of care.

Segments
The company operates through two segments, Evernorth Health Services and Cigna Healthcare.
Evernorth Health Services includes a broad range of coordinated and point solution health services and capabilities, as well as those from partners across the health care system, in Pharmacy Benefits, Home Delivery Pharmacy, Specialty Pharmacy, Distribution and Care Delivery and Management Solutions, which are provided to health plans, employers, government organizations and health care providers. Within Evernorth Health Services, Pharmacy Benefits and Home Delivery Pharmacy are foundational growth businesses and Specialty Pharmacy, Distribution, and Care Delivery and Management Solutions are accelerated growth businesses.
Cigna Healthcare includes the U.S. Commercial, U.S. Government and International Health operating segments, which provide comprehensive medical and coordinated solutions to clients and customers. Within Cigna Healthcare, U.S. Commercial and International Health are the company’s foundational growth businesses and U.S. Government is the company’s accelerated growth business.
Other Operations comprises the remainder of the company’s business operations, which includes certain ongoing businesses and exiting businesses. The company’s ongoing businesses include the company’s continuing business, corporate-owned life insurance (‘COLI’), and the company’s run-off businesses. The company’s run-off businesses include guaranteed minimum death benefit (‘GMDB’) and guaranteed minimum income benefit (‘GMIB’) business; settlement annuity business; and individual life insurance and annuity and retirement benefits businesses. The company’s exiting businesses include its interest in a joint venture in Türkiye, which was sold to the company’s partner in December 2022, the international life, accident and supplemental benefits businesses sold on July 1, 2022 and the Group Disability and Life business sold on December 31, 2020.
On July 1, 2022, the company completed the sale of its life, accident and supplemental benefits businesses in six countries (Hong Kong, Indonesia, New Zealand, South Korea, Taiwan and Thailand) to Chubb INA Holdings, Inc. (‘Chubb’).
Evernorth Health Services
Evernorth Health Services includes a broad range of coordinated and point solution health services and capabilities, as well as those from partners across the health care system, in Pharmacy Benefits, Home Delivery Pharmacy, Specialty Pharmacy, Distribution and Care Delivery and Management Solutions, which are provided to health plans, employers, government organizations and health care providers. These offerings are also integrated into the company’s Cigna Healthcare solutions to span the total health care delivery system.
On February 13, 2023, the company changed the name of the company’s Evernorth segment to Evernorth Health Services.
Evernorth Health Services accelerates delivery of comprehensive, connected solutions to create value and meet the diverse needs of health plans, employers, health care providers and government organizations by:
Partnering in unconventional ways to solve complex problems across a fragmented health care ecosystem, fueled by data and expertise that drives purposeful innovation.
Creating flexible solutions tailored to client needs, using Evernorth Health Services' combined strengths and capabilities, as well as strategic partnerships, to deliver: better, more efficient care for patients; better experiences for clients, providers and customers; and enhanced choices for clients and customers through the company’s open architecture model.
Evaluating medicines, digital therapeutics and other health solutions for efficacy, adherence, value and price to assist clients in selecting a cost-effective formulary.
Offering home delivery, virtual and in-person care, and specialty customer-centric solutions that meet the needs of the company’s clients and customers in ways that unlock greater value and better health services while providing better and specialized clinical care.
Delivering more affordable solutions that provide more discounts and drive risk-sharing and value-based care.
Promoting the use of generics and lowest-cost, clinically effective brands of medications.
Principal Products & Services
Pharmacy Benefits
Express Scripts Pharmacy dispenses approximately 1.6 billion adjusted prescriptions annually to members of pharmacy plans managed by the company’s Express Scripts PBM. The company drives high-quality, cost-effective care through prescription drug utilization and cost management services. The company supports its clients' plan design selections to deliver balanced affordability, choice, simplicity and convenience. The company focuses its solutions to align with its clients' service, care and cost management needs. As a result, the company delivers better care, healthier outcomes, higher customer satisfaction and a more affordable prescription drug benefit. The company dispenses drug claims via Express Scripts Pharmacy, Accredo and the company’s retail networks by integrating retail network pharmacy administration, benefit design consultation, drug utilization review, drug formulary management and pharmacy fulfillment services. The company administers payments to retail networks and bill benefits costs to the company’s clients through its end-to-end adjudication services.
Drug Utilization Review Program: When pharmacies submit claims for prescription drugs to the company, it reviews them electronically in real time for health and safety. The company then alerts the dispensing pharmacy of any detected issues. Clients may also choose to enroll in programs that result in communications about potential therapy concerns being sent to prescribers after the initial claim submission.
Benefits Design Consultation: The company consults with its clients on how best to structure and leverage the pharmacy benefit to meet plan objectives for affordable access to the prescription medications customers need to stay healthy and to ensure the safe and effective use of those medications.
myMatrixx: myMatrixx is a unique PBM with an exclusive focus on workers' compensation. The company combines high-touch customer service with clinical expertise and state-of-the-art business intelligence systems to deliver simplified solutions and positive outcomes. myMatrixx leverages Express Scripts' robust pharmacy network and provides a smooth and personalized experience for clients and injured workers.
Medical Drug Management: The company offers a comprehensive range of services and guaranteed savings for managing medically billed specialty drugs. The company’s solutions apply utilization management, site of care management and claims prepayment review to effectively reduce wasteful spend, while providing services tailored to customers ensuring safety and healthier outcomes. The company also offers Express Scripts MedRx Management, a suite of solutions and consultative services for medical rebates contracting, medically-billed drug preferencing and value-based contracting.
Embarc Benefit Protection: Embarc shields clients and members from the high costs of life-saving gene therapies, so that customers who need treatment can get it. Additionally, the program provides access to quality, cost-effective in-network providers and support from a dedicated gene therapy case management team.
FamilyPath: FamilyPath is raising the bar for fertility health by providing more comprehensive and more flexible coverage and proactive care for growing families, including expanded medical and pharmacy benefit management; access to vetted provider and lab networks; and dedicated Fertility Advisors to proactively support and guide customers.
Retail Network Pharmacy Administration: The company contracts with retail pharmacies to provide prescription drugs to customers of the pharmacy benefit plans the company manage. The company negotiates with pharmacies throughout the United States to discount drug prices provided to customers and manage national and regional networks responsive to client preferences related to cost containment, convenience of access for customers and network performance. The company also manages networks of pharmacies customized for or under direct contract with specific clients and has contracted with pharmacy provider networks to comply with the Center for Medicare and Medicaid Services (‘CMS’) access requirements for the federal Medicare Part D prescription drug program (‘Medicare Part D’). All retail pharmacies in the company’s network communicate with the company online and in real-time to process prescription drug claims.
Drug Formulary Management: Formularies are lists of drugs with designations that may be used to determine drug coverage, customer out-of-pocket costs and communicate plan preferences in competitive drug categories. The company’s formulary management services support clients in establishing formularies that assist customers and physicians in choosing clinically-appropriate, cost-effective drugs and prioritize access, safety and affordability. The company administers specific formularies on behalf of its clients, including standard formularies developed and offered by Express Scripts and custom formularies in which the company plays a more limited role. Most of the company’s clients select standard formularies, governed by the company’s National Pharmacy & Therapeutics Committee, which is consisted of a panel of independent physicians and pharmacists in active clinical practice representing a variety of specialties and practice settings, typically with major academic affiliations. In making formulary recommendations, this committee considers only the drug's safety and efficacy and not the cost of the drug, including any negotiated manufacturer discount or rebate arrangement. This process is designed to ensure the clinical recommendation is not affected by the company’s financial arrangements. The company fully complies with this committee's clinical recommendations regarding drugs that must be included or excluded from the formulary based on their assessment of safety and efficacy.
Advanced Utilization Management: These programs include prior authorization, drug quantity management and step therapy designed to decrease client spend on pharmacy.
Enhanced Fraud, Waste & Abuse: The company helps plan sponsors identify potential problem customers and prescribers with unusual or excessive utilization patterns. The program is designed to help identify outliers and situations of abnormal use or prescribing patterns by analyzing types of prescriptions, refill patterns and pharmacy utilization.
Administration of Group Purchasing Organizations: The company operates various group purchasing organizations that negotiate pricing for the purchase of pharmaceuticals and formulary rebates with pharmaceutical manufacturers on behalf of their participants. They also provide various administrative services to their participants including management and reporting.
Copay Solutions: The company’s first-to-market innovative copay solutions help customers afford their medications, protect plan design preferences and achieve lower trend. The company’s partnership with SaveOnSP on the first non-essential health benefits copay assistance solution has driven significant savings by targeting high-cost, high-volume drugs. SaveOnSP recommends plan design and coverage changes for certain drugs, enabling maximum savings and reducing plan and client costs. As manufacturer programs and regulations change, this aggressive solution adapts, delivering lower specialty plan cost and enhanced customer support.
Inside Rx: Inside Rx is a prescription medication savings program that offers eligible self-paying customers discounts on many brand and generic medications. This program is not insurance but offers savings at more than 60,000 participating retail pharmacies (including all major chains) in the United States and Puerto Rico. The program also offers discounts on prescription medications through private label solutions. Inside Rx earns a small fee from the company’s supply chain partners every time a customer fills a prescription via the program. This lets the company provide access to its savings card at no cost to the customer.
Evernorth Wholesale Marketplace: Evernorth Wholesale Marketplace offers a suite of flexible, private label solutions, including but not limited to Wholesale Marketplace Drug Formulary Management services, Retail Network Programs, Value-Based Solutions, Medical Rebate Programs and Utilization Management Policies. These offerings are captured under either the company’s drug formulary administrative service arrangements or its formulary processing arrangements. As the needs of the market evolve, the company will continue to partner with clients and develop additional offerings that align with their goals and objectives.
Value-Based Programs
Express Scripts SafeGuardRx: The company offers a solution platform aimed at therapy classes that pose budgetary threats and clinical challenges to customers. The company’s solutions are designed to keep its clients ahead of the drug cost curve while providing customers the personalized care and access they need. These solutions are offered throughout the company’s pharmacy benefit management services and include, but are not limited to care for: cardiovascular, diabetes, hepatitis, HIV, inflammatory conditions, neurological, multiple sclerosis, oncology, pulmonary, rare conditions and weight management. Innovative programs, such as Express Scripts SafeGuardRx, combine utilization management, formulary management, specialized care from the company’s Therapeutic Resource Centers and financial savings, to help the company to change the market in key categories. These services optimize the safe and appropriate dispensing of therapeutic agents, minimize waste and improve clinical and financial outcomes.
Express Scripts Patient Assurance Program: This program addresses affordability challenges for customers managing their diabetes and cardiovascular conditions by providing a lower, fixed, out-of-pocket cost directly to the customer. Express Scripts negotiates additional discounts to reduce customer cost share without increasing plan cost, and applies those discounts at the point of service. By making the cost of medication affordable and predictable, the Express Scripts Patient Assurance Program improves medication adherence, driving better customer outcomes and lower downstream medical costs for the plan.
Home Delivery Pharmacy: Evernorth Health Services offers free standard shipping of medications nationwide, usually in a 90-day supply, directly to the customer's home and allows for automatic refills on eligible medications and unrestricted telephone access to over 4,000 customer care advocates and specially trained pharmacists to answer customer questions. The company’s differentiated practice of pharmacy, coupled with its advanced automated dispensing technology, results in safer and more accurate pharmacy operations when compared to retail pharmacies, convenient access to maintenance medications and better management of the company’s clients' drug costs through operating efficiencies and generic substitutions. The company’s research shows that Express Scripts Pharmacy achieves a higher level of therapeutic interventions, better adherence, more cost savings and a consistently higher Net Promoter Score (marketplace ‘NPS’) compared to retail pharmacies. The Home Delivery Pharmacy operations consist of ten home delivery pharmacies and four high-volume automated dispensing pharmacies located throughout the United States. The company’s high-volume automated dispensing pharmacies are located in Arizona, Indiana, Missouri and New Jersey.
Specialty Pharmacy: Specialty medications are primarily characterized as high-cost medications for the treatment of complex and rare diseases. These medications broadly include those with frequent dosing adjustments, intensive clinical monitoring, the need for customer training, specialized product administration requirements or medications limited to certain specialty pharmacy networks by manufacturers. The front-end of the company’s pharmacy is organized into Therapeutic Resource Centers, where pharmacists focus their practice of pharmacy by condition, which offers customers a more personalized experience while providing enhanced clinical care. Through a combination of assets and capabilities, the company works to provide an enhanced level of predictable care and therapy management for customers taking specialty medications, leading to increased visibility and improved outcomes for payors and custom programs for biopharmaceutical manufacturers. The launch of biosimilars to blockbuster specialty therapies provides competition and an opportunity to drive down costs for both customers and clients. The company works with clients to efficiently support each benefit design to improve affordability. Accredo is focused on dispensing injectable, infused, oral and inhaled drugs that require a higher level of clinical service and support than traditional pharmacies typically offer. Accredo supports successful outcomes for customers and reduces waste for clients through specialty trained clinicians, a nationwide footprint and a network of in-home nursing services, reimbursement and customer assistance programs and biopharmaceutical services. Drug manufacturers may select Accredo for exclusive dispensing of highly specialized therapies. Freedom Fertility Pharmacy is dedicated exclusively to supporting customers undergoing fertility treatment. Accredo and Freedom Fertility Pharmacy serve customers within a pharmacy benefit plan administered by Express Scripts PBM, as well as customers in plans administered by other PBMs and health plans. The company’s Specialty Pharmacy operations consist of 33 specialty pharmacies.
Distribution: CuraScript SD is a specialty distributor of pharmaceuticals and medical supplies (including injectable and infusible pharmaceuticals and medications to treat specialty and rare or orphan diseases) directly to health care providers, clinics and hospitals in the United States for office or clinic administration. Through this business, the company provides distribution services primarily to office and clinic-based physicians who treat customers with chronic diseases and regularly order costly specialty pharmaceuticals. This business provides competitive pricing on pharmaceuticals and medical supplies, operates three distribution centers and ships most products overnight within the United States; it also provides distribution capabilities to Puerto Rico and Guam. It is a contracted supplier with most major group purchasing organizations and leverages the company’s distribution platform to operate as a third-party logistics provider for several pharmaceutical companies.
Care Delivery and Management Solutions: The company offers clinical programs to help its clients drive better whole-person health outcomes through the company’s Care Delivery (virtual care, in-home care, physical primary care) and Care Management (behavioral health services and health coaching capabilities) offerings.
eviCore: eviCore healthcare is a medical benefits management organization that is a leading provider of solutions that ensure customers receive optimal treatment at the right site of care by leveraging the company’s team of medical professionals, evidence-based guidelines and innovative technologies to deliver affordable care. eviCore provides integrated solutions for key clinical diagnostic areas, such as advanced imaging, cardiology and gastroenterology, as well as longitudinal areas, such as musculoskeletal, oncology and post-acute care. eviCore contracts with health plans to promote the appropriate use of health care services by the customers they serve. In certain instances, this occurs through capitated risk arrangements, when the company assumes the financial obligation for the cost of health care services provided to eligible customers covered by eviCore healthcare management programs.
MDLIVE: MDLIVE virtual care services provide flexibility for the customer to access a network of virtual care providers for preventative and routine primary care and wellness, urgent care, dermatology care, behavioral health care needs and chronic condition management beginning with hypertension.
Behavioral Health: The company’s behavioral health solutions simplify the complicated treatment landscape by assisting members to the right level of care at the right time, in the right place - from start to finish. The company’s predictive analytics models proactively identify customers who need support so that the company can engage them early and provide the appropriate care, leveraging its extensive provider network, including in-person providers, virtual providers and digital tools.
inMynd: The company’s Evernorth inMynd Behavioral Health and inMyndRx solutions provide access to expert guidance and support for anxiety, depression, insomnia, ADHD, narcolepsy, Alzheimer's and select mood stabilizing medications. These solutions include providing access to individualized support and educational resources, condition-specific care through the company’s Neuroscience Therapeutic Resource Centers and digital Cognitive Behavioral Therapy program when applicable.
Health Connect 360: This program is a transformational, outcomes-based, clinical management model that bridges pharmacy, medical, lab and biometric data to develop insights and deliver personalized health care clinical support. Clinical outcomes and quality metrics are tailored to meet client needs.
RationalMed: RationalMed improves customer health and safety by integrating medical, pharmacy and laboratory claims data to initiate changes and correct errors in care, lowering both medical and prescription drug costs.
Evernorth Digital Health Formulary: Through the Evernorth Digital Health Formulary, the company evaluates, procures, implements and manages digital health solutions on behalf of clients, alleviating administrative burden and ensuring clinical effectiveness, data security, user-friendly experiences and financial value.
Cigna Pathwell Specialty: Cigna Pathwell Specialty is designed to address one of the company’s clients' top health care cost drivers - specialty drugs - enabling clients to reinvest in their employees, making health care more affordable. This new solution controls specialty spending across the medical and pharmacy benefits by integrating pharmacy network and care coordination for customers who need the company’s support the most.
Evernorth Intelligence Solutions: By bringing together world-class talent, multi-disciplinary expertise and advanced data and analytics, the company unlocks actionable insights to help drive greater affordability, simplicity, predictability and growth. The company works together with its clients and partners to create dynamic solutions, services and platforms that guide better decisions and improved performance.
Evernorth Labs: The company accelerates innovation through increased collaboration with clients, customers and partners to develop solutions for launch in their businesses. With the company’s Labs, which are state-of-the-art research facilities and shared spaces for collaboration, ideation and innovation, the company gathers with its clients and industry leaders to solve the toughest challenges in the health care system, including better managing the most complex and expensive disease states, such as oncology; improving care access and delivery, such as worksite, home and virtual care; and planning for emerging trends, such as artificial intelligence, and industry disruptors, such as COVID-19.
Data, Advanced Analytics and Platforms: The company uses advanced predictive modeling to shape solutions that help decrease health care fragmentation, drive optimized care coordination, reduce key cost drivers and improve health outcomes. In-depth trend analysis helps the company to identify and effectively address challenges like opioid abuse, COVID-19 and other emerging health crises. The company uses market surveillance and forecasting to pinpoint and proactively address cost drivers. The company’s platform strategy as a service gives clients the tools to build successful businesses in a flexible, customizable way: Trend Central provides access to key performance indicators to help plan sponsors reduce costs and work towards healthier outcomes; HealthPredict produces high customer-level risk scores, to show the highest value opportunities for proactive intervention; MediCUBE gives the company’s academic detailing pharmacists the analytical power to identify ways to save plans from significant unnecessary spend and improve quality metrics; and ScriptVision provides a suite of real-time, data-driven capabilities that empower physicians to make the best prescribing choices, including ePrescribing (including controlled substances), real-time prescription benefit information, electronic prior authorizations, clinical care messages, such as drug interactions and high-risk medication alerts and data on customer adherence rates.
Customers
The company provides products and services in the Evernorth Health Services segment to clients and customers, as described below. Also described below are the company’s significant clients.
Clients: The company provides services to managed care organizations, health insurers, third-party administrators, employers, union-sponsored benefit plans, workers' compensation plans, government health programs, providers, clinics, hospitals and others. The company provides services to a majority of customers in the company’s Cigna Healthcare segment.
Customers: Prescription drugs are dispensed to patients connected to the service offerings the company provide to clients. Prescription drugs are dispensed primarily through networks of retail pharmacies under non-exclusive contracts with the company and via home delivery from Express Scripts Pharmacy and specialty drug fulfillment pharmacies.
The Department of Defense (‘DoD’) TRICARE Pharmacy Program is the military health care program serving active-duty service customers, National Guard and Reserve customers and retirees, as well as their dependents. Under this contract, the company provides online claims adjudication, home delivery services, specialty pharmacy clinical services, claims processing and contact center support and other services critical to managing pharmacy trend. In 2021, the DoD awarded Express Scripts a seven-year pharmacy program contract beginning January 1, 2023. Under the new contract, Express Scripts will provide enhanced specialty care and expanded care coordination capabilities, while continuing to support current pharmacy operations, through 2029.
In 2019, Express Scripts and Prime Therapeutics LLC (‘Prime’) entered into an agreement effective on April 1, 2020 to deliver improved choice and affordability for Prime's clients and their customers by enhancing retail pharmacy networks and pharmaceutical manufacturer value. In 2022, Prime and Express Scripts agreed to extend this relationship through 2025. In 2021, the relationship with Prime was expanded to include the option for Prime's plans to access the Accredo specialty pharmacy and Express Scripts home delivery in-network pharmacies.
In October 2022, Evernorth Health Services and Centene Corporation (‘Centene’) announced a multi-year agreement effective January 2024 to manage pharmacy benefit services and make prescription medications more accessible and affordable for Centene's approximately 20 million customers. In addition to greater savings on prescription drugs, Centene customers will also have access to Express Scripts' extensive national network of retail pharmacies.
Competition
Managed Care PBMs: CVS Caremark (owned by CVS Health Corporation (‘CVS’)), Humana Inc. (‘Humana’), IngenioRx (owned by Elevance Health Inc. (‘Elevance’)), OptumRx (owned by UnitedHealth Group Inc. (‘UnitedHealth’)) and Prime Therapeutics (owned by a collection of Blue Cross / Blue Shield Plans) compete with the company on a variety of products and in various regions throughout the United States.
Independent PBMs: MedImpact, Navitus Health Solutions, Elixir (owned by Rite Aid Corporation) and many other regional PBMs compete with the company on a variety of products across the United States.
Pharmacies: CVS, Walgreens Boots Alliance, Inc., WalMart, Inc., Rite Aid, Kroger and other independent pharmacies compete with the company for the delivery of prescription drug needs to the company’s customers. In addition, many PBMs own and operate home delivery and specialty pharmacies, including CVS, OptumRx, Walgreens, Humana and Elixir. New entrants continue to emerge, including Amazon Pharmacy, Capsule and Hims.
Third-Party Benefits Administrators: Third parties that specialize in claim adjudication and benefit administration, such as SS&C Health, are direct competitors.
Care Delivery and Management Solutions: OptumHealth, NaviHealth and Landmark (UnitedHealth); Beacon, Aspire and CareMore (owned by Elevance); CVS's HealthHubs and MinuteClinics; CenterWell Home Health (Humana); Community and Bayless (Centene); VillageMD, Teladoc, Doctor on Demand, MeMD, WalmartHealth and AmazonCare are among the companies that compete with the company in this market.
Clinical Solutions and Health Care Data Analytics Companies. Optum (owned by UnitedHealth), Elevance, Magellan Health and Apixio (owned by Centene Corporation), HealthHelp, Cotiviti and Inovalon are among the companies that compete with the company in this market.
Operations
Sales and Account Management: The company’s sales and account management teams market and sell pharmacy benefit management solutions and are supported by client service representatives, clinical pharmacy managers and benefit analysis consultants. These teams work with clients to develop innovative strategies that put medicine within reach of customers while helping health benefit providers improve access to and affordability of prescription drugs.
Supply Chain: The company’s supply chain contracting and strategy teams negotiate and manage pharmacy retail network contracts, pharmaceutical and wholesaler purchasing contracts and manufacturer rebate contracts. As the company’s clients continue to experience increased cost trends, the company’s supply chain teams develop innovative solutions, such as the company’s Express Scripts SafeGuardRx platform and preferred pharmacy networks to combat these cost increases. In addition, the company’s Formulary Consulting team, consisting of pharmacists and financial analysts, provides services to the company’s clients to support formulary decisions, benefit design consultation and utilization management programs.
Clinical Support: The company’s staff of highly trained health care professionals provides clinical support for the company’s pharmacy, medical and behavioral customers. The company’s services include access to:
Support for the individual and their caregivers from crisis care in their most vulnerable moments to stabilization and returning back to work and life for all involved.
Comprehensive behavioral health offerings including network access, utilization management and coordination of care to treat conditions ranging from depression and anxiety to substance use, autism and eating disorders.
Condition-specific specialized customer care through the company’s Therapeutic Resource Center facilities staffed with specialist pharmacists, nurses and other clinicians.
Clinical development and operational support for the company’s pharmacy benefit management services by the company’s clinical solutions staff of pharmacists and physicians who conduct a wide range of activities including: identifying emerging medication-related safety issues and alerting physicians, clients and customers (as appropriate); providing drug information services; managing formulary; identifying and closing gaps in care; and developing utilization management, safety (drug utilization review) and other clinical interventions.
Cigna Healthcare segment
Cigna Healthcare segment includes the U.S. Commercial, U.S. Government, and International Health operating segments, which provide comprehensive medical and coordinated solutions to clients and customers. Within Cigna Healthcare, U.S. Commercial and International Health are the company’s foundational growth businesses and U.S. Government is the company’s accelerated growth business.
By offering a mix of services and medical insurance products to employers, groups and individuals along with specialty products, the company improves the quality of care, lower costs and help customers achieve better health outcomes. Many of these products are available on a standalone basis, but they create additional value and savings when integrated with a Cigna Healthcare-administered health plan.
Principal Products & Services
U.S. Commercial Medical
Managed Care Plans are offered through the company’s insurance companies, Health Maintenance Organizations (‘HMOs’) and TPA companies. HMO, LocalPlus, Network and Open Access Plus plans use meaningful cost-sharing incentives to encourage the use of ‘in-network’ versus ‘out-of-network’ health care providers. The national provider network for Managed Care Plans is smaller than the national network used with the PPO plan product line.
PPO Plans feature a network with broader provider access than the Managed Care Plans.
Consumer-Driven Products are typically paired with a high-deductible medical plan and offer customers a tax-advantaged way to pay for eligible health care expenses. These products, consisting of health savings accounts, health reimbursement accounts and flexible spending accounts, encourage customers to play an active role in managing their health and health care costs.
U.S. Government Medical
Individual and Family Plans are Patient Protection and Affordable Care Act (‘ACA’) compliant exclusive provider organization (‘EPO’) or HMO plans marketed to individuals under age 65 who do not have access to health care coverage through an employer or government program, such as Medicare or Medicaid. Customers receive comprehensive health care benefits and have access to a local network of health care providers who have been selected with cost and quality in mind.
Medicare Advantage Plans allow Medicare-eligible customers to receive health care benefits, including prescription drugs, through a managed care health plan, such as the company’s coordinated care plans. The company’s Medicare Advantage Plans include HMO and PPO plans marketed to individuals and qualified employer groups. A significant portion of the company’s Medicare Advantage customers receive medical care from the company’s value-based models that focus on developing highly engaged physician networks, aligning payment incentives to improve health outcomes and using timely and transparent data sharing.
Medicare Stand-Alone Prescription Drug (‘Part D’) Products provide a number of prescription drug plan options, as well as service and information support to Medicare-eligible individuals or individuals through a qualified employer group. The company’s stand-alone plans offer the coverage of Medicare combined with the flexibility to select a product that provides enhanced benefits and a formulary that aligns with the individual's needs. Eligible customers benefit from broad network access and enhanced service intended to promote adherence, wellness and affordability.
Medicare Supplement Plans provide Medicare-eligible customers with federally standardized Medigap-style plans. Customers may select among the various plans with specific plan options to meet their unique needs and may visit, without the need for a referral, any health care provider or facility that accepts Medicare throughout the United States.
Specialty Products and Services
Stop-Loss insurance coverage is offered to self-insured clients whose group health plans are administered by Cigna Healthcare. Stop-loss insurance provides reimbursement for claims in excess of a predetermined amount for individuals, the entire group, or both.
Cost Containment Programs are designed to contain the cost of covered health care services and supplies. These programs reduce out-of-network utilization and costs, protect customers from balance billing and educate customers regarding the availability of lower cost in-network services. In addition, under these programs the company negotiate discounts with out-of-network providers, review provider bills and recover overpayments. The company charges fees for providing or arranging for these services. These programs may be administered by third-party vendors that have contracted with Cigna Healthcare.
Consumer Health Engagement services are offered to customers covered under plans administered by Cigna Healthcare or by third-party administrators. These services consist of an array of health management, disease management and wellness services. The company’s Medical Management programs include case, specialty and utilization management and a 24/7 Health Information line which ensures around the clock access to a medical professional. The company’s Health Advocacy program services include early intervention in the treatment of chronic conditions and an array of health and wellness coaching. The company administers incentives programs designed to encourage customers to engage in health improvement activities.
Pharmacy Management services and benefits can be combined with the company’s medical offerings. The comprehensive suite of pharmacy management services is available to clients and customers through the company’s integration with Evernorth Health Services' capabilities.
Behavioral Health services consist of a broad national network of behavioral health providers, which includes one of the largest virtual networks in the United States, behavioral health specialty case and utilization management, a crisis intervention line accessible anytime, employee assistance programs and work/life programs. The company integrates its programs and services with medical and pharmacy programs to facilitate customized, holistic care, as well as to provide resources that increase resiliency and address non-medical factors that affect overall well-being.
Dental solutions include dental HMO plans, dental PPO plans, exclusive dental provider organization plans, traditional dental indemnity plans, and a dental discount program. Employers and other groups can purchase the company’s products on either an insured or self-insured basis as standalone products or in conjunction with medical products. Additionally, individual customers can purchase insured dental PPO plans as standalone products or in conjunction with individual medical policies.
International Health
Global Health Care products and services include insurance and administrative services for medical, dental, pharmacy, vision and life, accidental death and dismemberment and disability risks. The company is a leading provider of products and services that meet the needs of multinational employers, intergovernmental and nongovernmental organizations and globally mobile individuals with a focus on keeping employees healthy and productive. The employer benefits products and services are offered through guaranteed cost, experience-rated and administrative services only funding solutions, while individuals purchase guaranteed cost coverage.
Local Health Care products and services include medical, dental, pharmacy and vision as well as life coverage. The customers of local health care businesses are employers and individuals located in specific countries where the products and services are purchased. These employer services can similarly be funded through a range of options; individuals purchase on a guaranteed cost basis.
Market Segments
U.S. Commercial comprises the following market segments:
National: Employers with 3,000 or more eligible employees, primarily through ASO funding solutions.
Middle Market: Employers generally with 500 to 2,999 eligible employees, solutions for third party payers, Taft-Hartley plans, as well as other groups, through ASO and insured funding solutions.
Select: Employers generally with 51 to 499 eligible employees, primarily through ASO with stop-loss insurance coverage and insured funding solutions.
Small Group: Employers generally with 2 to 50 eligible employees. The company offers guaranteed cost insured funding solutions in select geographies with the company’s Cigna + Oscar product.
U.S. Government comprises the following market segments:
Individual: Includes individuals under age 65 who do not have access to health care coverage through an employer or government program, such as Medicare or Medicaid. The company offers guaranteed cost, medical ACA-compliant and dental plans in this market segment.
Medicare: Includes individuals who are Medicare-eligible customers, as well as employer group sponsored post-65 retirees. The company receives Medicare Advantage revenue from CMS based on customer demographic data and health risk factors.
International Health comprises market segments offering international plans to multinational employers and globally mobile individuals, and domestic plans to employers and individuals in specific countries outside of the U.S. Employer plans in the International Health segment may be ASO or fully insured plans.
Customers
The company provides clients and customers with access to a mix of medical and specialty products and services.
Clients: The company’s clients include employers, third-party administrators, union-sponsored benefit plans, government health programs and other groups which span the company’s operating segments.
Customers: The company’s customers include individuals who access the company’s offerings through an employer-sponsored plan, government-sponsored plan, or other insured group.
Primary Distribution Channels
Brokers: Sales representatives distribute the company’s products and services to a broad group of insurance brokers and consultants.
Direct: Cigna Healthcare sales representatives distribute the company’s products and services directly to employers, unions and other groups or individuals. Various products may also be sold directly to insurance companies, HMOs and third-party administrators. Direct distribution may take the form of in-person contact, telephone or group selling venues, or online direct to consumer enrollment platforms.
Private Exchanges: The company partners with select companies that have created private exchanges where individuals and organizations can acquire health insurance. The company evaluates private exchange participation opportunities as they emerge in the market and target the company’s participation to those models that best align with the company’s mission and value proposition.
Public Exchanges: Cigna Healthcare offers individual ACA-compliant policies through public health insurance exchanges in select geographies.
Competition
National Insurers: UnitedHealth, Aetna Inc. (owned by CVS), Elevance, Humana and Blue Cross Blue Shield plans compete with the company in a variety of products and regions.
Local Healthplans: Blue Cross Blue Shield plans, local affiliates of major insurance companies and hospitals and regional stand-alone managed care and specialty companies compete with the company in the states in which the company offers managed care products.
Partnering to Advance Growth Strategy
Cigna Healthcare's strategy engages customers in their health, collaborates with providers to help them improve their performance and connects customers and providers through aligned health goals, incentives and actionable information to help enable informed decisions and drive better outcomes. Continuing to expand the breadth and depth of Evernorth Health Services care services, pharmacy services and benefits management will further reduce the total cost of care for the company’s clients and customers. Fueled by advanced insights and predictive analytics, Cigna Healthcare continues to develop innovative solutions that span the health care delivery system and can be applied to a multitude of providers.
Accountable Care Program: The company has approximately 239 collaborative care arrangements with primary care groups built on the patient-centered medical home and accountable care organization (‘ACO’) models. Program flexibility allowed adjustments in response to the COVID-19 pandemic designed to maintain appropriate focus on high-risk individuals and populations with chronic conditions impacted by Social Determinants of Health. As the company emerge from the pandemic, the company is leveraging new models to increase provider adoption of upside and downside risk sharing to drive better health outcomes and lower the total cost of care.
Hospital Quality Program: The company has contracts with approximately 152 hospital systems, involving over 592 hospitals, with reimbursements tied to quality metrics.
Site of Care Redirection: The company encourages the use of clinically appropriate settings to reduce the cost of care. This results in significant cost savings compared to receiving the same care in a hospital setting, while ensuring high quality care and service.
Specialist Programs: The company has approximately 266 arrangements with specialist groups in value-based reimbursement arrangements across six different disciplines. Arrangements include incentives for enhanced care coordination and episodes of care reimbursements for meeting cost and quality goals. The company has expanded these programs to include prospective bundled payment arrangements beginning with orthopedics.
Independent Practice Associations: The company has value-based physician engagement models in the company’s Medicare Advantage plans that allow physician groups to share financial outcomes with the company. This clinical model also includes outreach to new and at-risk patients to ensure they are accessing their primary care physician.
Participating Provider Network: The company provides its customers with an extensive network of participating health care providers, hospitals and other facilities, pharmacies and providers of health care services and supplies. In addition, the company has strategic alliances with several regional managed care organizations to gain access to their provider networks and discounts.
Virtual Care: The company encourages access for customers through MDLIVE telehealth services as a way to support the patient/provider relationship. MDLIVE telehealth services provide flexibility for the customer to access a network of telehealth providers for services, including preventative and routine primary care and wellness, urgent care, dermatology care, behavioral health care needs and chronic condition management beginning with hypertension.
Other Operations
Other Operations comprises the remainder of the company’s business operations, which includes certain ongoing businesses and exiting businesses. The company’s ongoing businesses include the company’s continuing business, COLI, as described below, as well as the company’s run-off businesses. The company’s run-off businesses include GMDB and GMIB business that were effectively exited through reinsurance with Berkshire Hathaway Life Insurance Company of Nebraska (‘Berkshire’) in 2013; settlement annuity business; and individual life insurance and annuity and retirement benefits businesses consisted of deferred gains from the sale of these businesses. The company’s exiting businesses include the company’s interest in a joint venture in Türkiye, which was sold to the company’s partner in December 2022, the international life, accident and supplemental benefits businesses sold on July 1, 2022, and the Group Disability and Life business sold on December 31, 2020.
Ongoing Businesses
Continuing Business
Corporate-Owned Life Insurance
The principal products of the COLI business are permanent insurance contracts sold to corporations to provide coverage on the lives of certain employees for financing employer-paid future benefit obligations. Permanent life insurance provides coverage that, when adequately funded, does not expire after a term of years. The contracts are primarily non-participating universal life policies. Fees for universal life insurance products consist primarily of mortality and administrative charges assessed against the policyholder's fund balance. Interest credited and mortality charges for universal life and mortality charges on variable universal life may be adjusted prospectively to reflect expected interest and mortality experience. To reduce the company’s exposure to large individual losses, the company purchases reinsurance from unaffiliated reinsurers.
Run-off Businesses
Settlement Annuity Business
The company’s settlement annuity business is a closed, run-off block of single premium annuity contracts. These contracts are primarily liability settlements with approximately 15% of the liabilities associated with guaranteed payments not contingent on survivorship. Non-guaranteed payments are contingent on the survival of one or more parties involved in the settlement.
Reinsurance
The company’s reinsurance operations are an inactive business in run-off.
In February 2013, the company effectively exited the GMDB and GMIB business by reinsuring 100% of the company’s future exposures, net of retrocessional arrangements in place at that time, up to a specified limit.
Individual Life Insurance and Annuity and Retirement Benefits Businesses
Exiting Businesses
The company’s Interest in a Joint Venture in Türkiye.
In December 2022, the company divested its ownership interest in Cigna Saglik Hayat ve Emeklilik, the company’s joint venture in Türkiye, to the company’s long-time partner QNB Finansbank.
International Life Accident and Supplemental Benefits
The company offered life, accident and supplemental benefits insurance products and services in Hong Kong, Indonesia, New Zealand, South Korea, Taiwan and Thailand until the completion of the sale of these businesses on July 1, 2022 to Chubb.
Group Disability and Life
The company’s Group Disability and Life operating segment included the company’s commercial long-term and short-term disability products and the company’s term life group insurance products, until completion of the sale in 2020. The company also offered personal accident insurance and will continue to offer voluntary products and services that were not part of the sale. Beginning in 2021, voluntary products and services are reported in the Cigna Healthcare segment.
Investment Management
The company’s investment operations provide investment management and related services for the company’s various businesses, including the insurance-related invested assets in the company’s General Account (‘General Account Invested Assets’). The company acquires or originates, directly or through intermediaries, a broad range of investments, including private placement and public securities, commercial mortgage loans, real estate, mezzanine, private equity partnerships and short-term investments.
Separate Accounts
The company’s subsidiaries or external advisors manage invested assets of separate accounts on behalf of contract holders, including The Cigna Group Pension Plan, variable universal life products sold through the company’s corporate-owned life insurance business and other life insurance products. These assets are legally segregated from the company’s other businesses and are not included in General Account Invested Assets.
Strategic Investments
Cigna Ventures: In addition to the portfolio investments in the company’s general and separate accounts discussed in the Investment Management section above that support the company’s insurance operations, the company makes targeted investments within the health care industry, specifically. Cigna Ventures invests in promising startups and growth-stage companies who, like the company, are unlocking new growth possibilities in health care. Specifically, the company invests in companies making groundbreaking progress in three strategic areas: insights and analytics, digital health and experience, and care delivery and enablement. As of December 31, 2022, Cigna Ventures had seven venture capital partners and 22 existing direct investments. Through these deep partnerships the company collaborates, innovates and develops new solutions that address critical challenges of health and vitality impacting the people the company serves.
VillageMD: As of December 31, 2022, the company had a commitment to become a minority owner in VillageMD by investing in VillageMD preferred equity. VillageMD is an independent primary care group committed to offering high-quality, accessible primary care options for communities across the country through Village Medical. VillageMD partners with physicians to provide the tools, technology, operations, staffing support and industry relationships to deliver high-quality clinical care and better patient outcomes. VillageMD and Village Medical operate in 22 markets and are responsible for more than 1.6 million patients.
Intellectual Property Rights
The company holds over 320 United States patents.
Regulation
Many aspects of the company’s business are directly regulated by federal and state laws and administrative agencies, such as HHS, CMS, the Internal Revenue Service (‘IRS’), the U.S. Departments of Labor (‘DOL’) and Treasury, the Office of Personnel Management (‘OPM’), the Federal Trade Commission (‘FTC’), the SEC, the Office of the National Coordinator for Health Information Technology (‘ONC’), state departments of insurance and state boards of pharmacy.
The company’s business operations and the books and records of its regulated businesses are routinely subject to examination and audit at regular intervals by state insurance and HMO regulatory agencies, state boards of pharmacy, CMS, DOL, IRS, OPM and comparable international regulators to assess compliance with applicable laws and regulations. The company’s operations are also subject to non-routine examinations, audits and investigations by various state and federal regulatory agencies, generally as the result of a complaint. As a result, the company routinely receives subpoenas and other demands or requests for information from various state insurance and HMO regulatory agencies, state attorneys general, the HHS Office of Inspector General (HHS-OIG), the DOJ, the DOL and other state, federal and international authorities.
The company’s business model is impacted by the Patient Protection and Affordable Care Act, including its relationships with producers and health care providers, products, service providers and technologies.
Through the company’s subsidiaries, it offers individual and group Medicare Advantage, Medicare Prescription Drug (‘Part D’) and Medicare Supplement products. The company also provides Medicare Part D-related products and services to other Medicare Part D sponsors, Medicare Advantage Prescription Drug Plans and employers and clients offering Medicare Part D benefits to Medicare Part D eligible beneficiaries, including those dually eligible for Medicare and Medicaid benefits (‘dual-eligible’). As part of the company’s Medicare Advantage and Medicare Part D business, the company contracts with CMS to provide services to Medicare beneficiaries. The company offers dual-eligible products and participates in state Medicaid programs directly or indirectly through its clients who are Medicaid managed care contractors. The company also performs certain Medicaid subrogation services and certain delegated services for clients, including utilization management, which are regulated by federal and state laws. The company’s dual-eligible products are regulated by CMS and state Medicaid agencies audit its performance to determine compliance with contracts and regulations.
The company’s products and services are also subject to the federal False Claims Act (the ‘False Claims Act’), state false claims acts and federal and state anti-kickback laws.
The DOJ is also conducting industry-wide investigations of the risk adjustment data submission practices and business processes of the company and a number of other Medicare Advantage organizations.
The company has a contract with the U.S. DoD, which subjects the company to applicable Federal Acquisition Regulations (FAR) and the DoD FAR Supplement, which govern federal government contracts. In addition, certain of the company’s clients participate as contracting carriers in the Federal Employees Health Benefits Program administered by the OPM, which includes various pharmacy benefit management standards.
The company’s domestic subsidiaries sell most of their products and services to sponsors of employee benefit plans that are governed by ERISA.
The company is also subject to the Payment Card Industry Data Security Standard, a set of requirements designed to help ensure that entities that Process credit card information maintain a secure environment.
On the federal level the company is subject to a number of sector specific regulation. The federal Health Insurance Portability and Accountability Act of 1996, the Health Information Technology for Economic and Clinical Health Act, the 21st Century Cures Act, Public Law 116-321, and the regulations that implement these laws (collectively ‘HIPAA’) impose requirements on covered entities and business associates that address the privacy and security of PHI.
The company is therefore subject to federal and state regulations applicable to electronic communications and other consumer protection laws and regulations, such as the Telephone Consumer Protection Act and the CAN-SPAM Act.
The company is also subject to regulation by the Office of Foreign Assets Control of the U.S. Department of the Treasury, which administers and enforces economic and trade sanctions against targeted foreign countries and regimes based on the U.S. foreign policy and national security goals. Certain of the company’s products are subject to the Department of the Treasury anti-money laundering regulations under the Bank Secrecy Act. In addition, the company is subject to similar regulations in non-U.S. jurisdictions in which the company operates.
The company’s home delivery and specialty pharmacies also subject it to extensive federal, state and local regulation. The practice of pharmacy is generally regulated at the state level by state boards of pharmacy, though the company’s pharmacies are subject to laws described above under the headings ‘Privacy, Security and Data Standards Regulations’ and ‘Consumer Protection Laws’.
Additionally, the company is subject to CMS rules regarding the administration of its Medicare plans and pricing between its plans and related parties, including its pharmacy business.
Federal and state statutes and regulations govern the labeling, packaging, repackaging, compounding, storing, holding, disposal, distribution, advertising, misbranding, adulteration, transfer, handling and security of prescription drugs and the dispensing of prescription, over-the-counter, hazardous and controlled substances and certain of the company’s pharmacies must register with the U.S. Drug Enforcement Administration, the U.S. Food and Drug Administration, and individual state controlled substance authorities.
The company’s operations in countries outside of the United States are subject to local regulations of the jurisdictions where it operates; in some cases, are subject to regulations in the jurisdictions where customers reside; and in all cases, are subject to the Foreign Corrupt Practices Act (FCPA).
History
Cigna Corporation was founded in 1792. The company was incorporated in the state of Delaware in 1981.

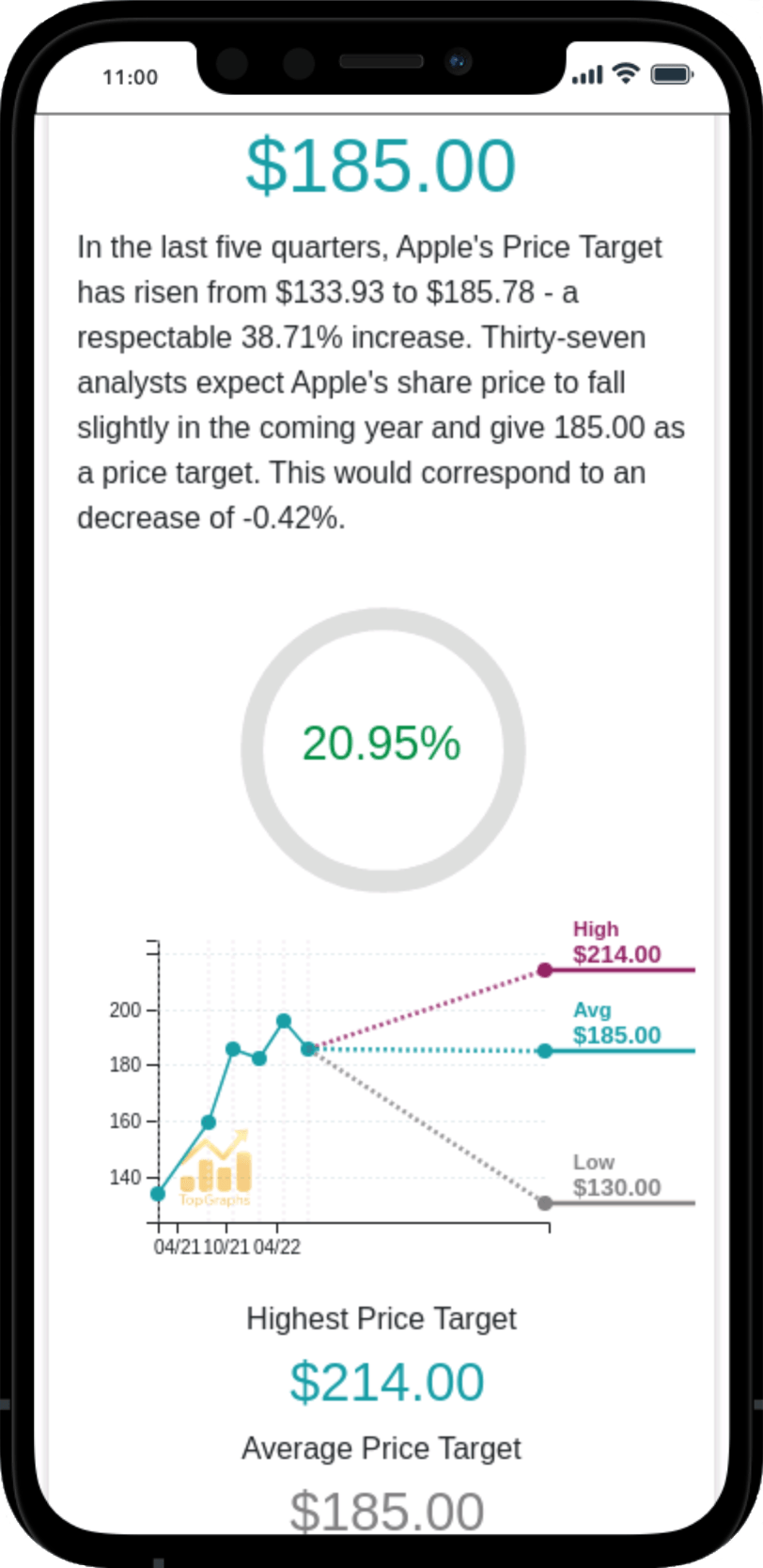
 Stock Value
Stock Value